Patterns, Predictors, and Prognostic Implication of Treatment-Related Amenorrhea in Patients With Breast Cancer
DOI:
https://doi.org/10.14740/wjon1991Keywords:
Breast cancer, Treatment-related amenorrhea, Risk factors, SurvivalAbstract
Background: Treatment-related amenorrhea (TRA) is a common side effect of treatment in premenopausal patients with breast cancer, with important consequences for patient counseling and management. Its occurrence and potential influence on survival outcomes remain active areas of investigation. This study aimed to evaluate the incidence, risk factors, and prognostic significance of TRA in patients with breast cancer.
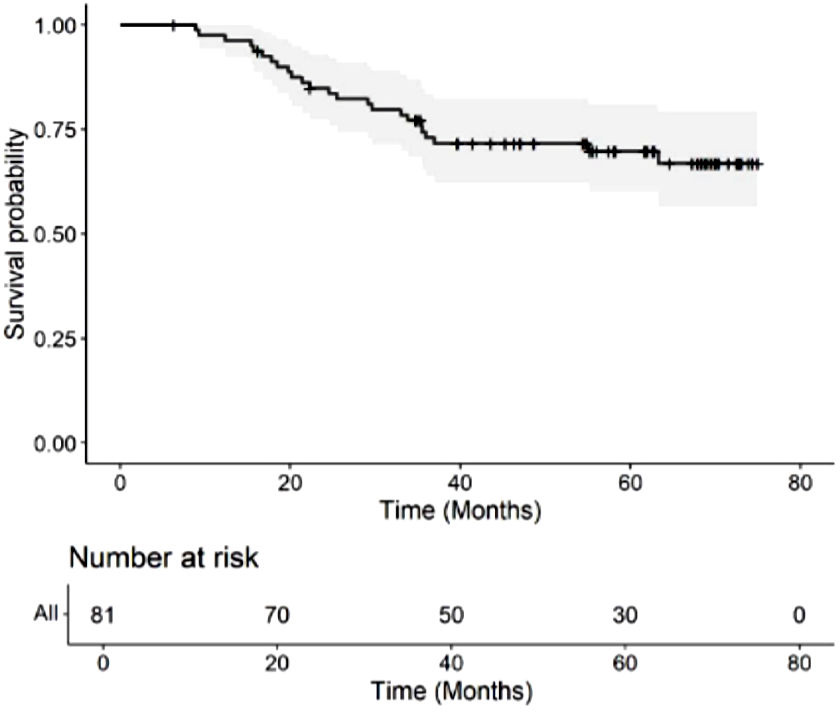
Methods: This is a retrospective cohort study. Patients were interviewed during and after chemotherapy to assess their menstrual status. Sociodemographic, clinical, and treatment data of patients were also collected. TRA was classified into early amenorrhea (EA) and late amenorrhea (LA) based on the duration of amenorrhea. Univariable and multivariable logistic regression were used to identify risk factors of EA and LA. Kaplan-Meier curves and Cox proportional hazards analyses were used to investigate the impact of EA and LA on 3-year overall survival (OS).
Results: There were 81 patients who were eligible for the final analysis. Of these subjects, 14 (17.3%) developed no amenorrhea, 67 (82.7%) developed EA, and 45 (55.6%) developed LA. We did not find any significant independent risk factor for EA. Age > 45 years (odds ratio (OR): 4.00; confidence interval (CI): 1.23 - 13.01; P = 0.021) and the usage of hormonal therapy (OR: 4.96; CI: 1.58 - 15.53; P = 0.006) independently significantly increase the risk of LA, whereas a metastatic disease status decreased the risk (OR: 0.20; CI: 0.04 - 0.90; P = 0.036). Both EA (hazard ratio (HR) = 0.262, CI: 0.105 - 0.653; P = 0.002) and LA (HR = 0.234, CI: 0.091 - 0.604; P = 0.001) were associated with an improved 3-year OS rate.
Conclusions: Age > 45 years and the usage of hormonal therapy are risk factors for LA, while metastatic disease was associated with a decreased risk. Both EA and LA had a significant association with favorable 3-year OS. These findings enable clinicians to provide personalized guidance, tailor treatment strategies, and improve the outcomes of premenopausal patients with breast cancer. Standardization of how TRA is defined and assessed in future studies is essential to improve comparability and enhance the understanding of its clinical implications.
Published
Issue
Section
License
Copyright (c) 2024 The authors

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.