Time-to-Treatment Initiation and Its Effect on All-Cause Mortality: Insights From the Surveillance, Epidemiology, and End Results Database
DOI:
https://doi.org/10.14740/wjon2584Keywords:
Mortality, Time-to-treatment initiation, Breast cancer, Lung cancer, Prostate cancer, Colorectal cancerAbstract
Background: Delays in cancer treatment initiation can significantly impact survival outcomes, but the magnitude of this effect varies by cancer type, stage, and patient demographics. This study examined the association between time-to-treatment initiation (TTI) and all-cause mortality across multiple common cancers, evaluating differential impacts and sociodemographic disparities.
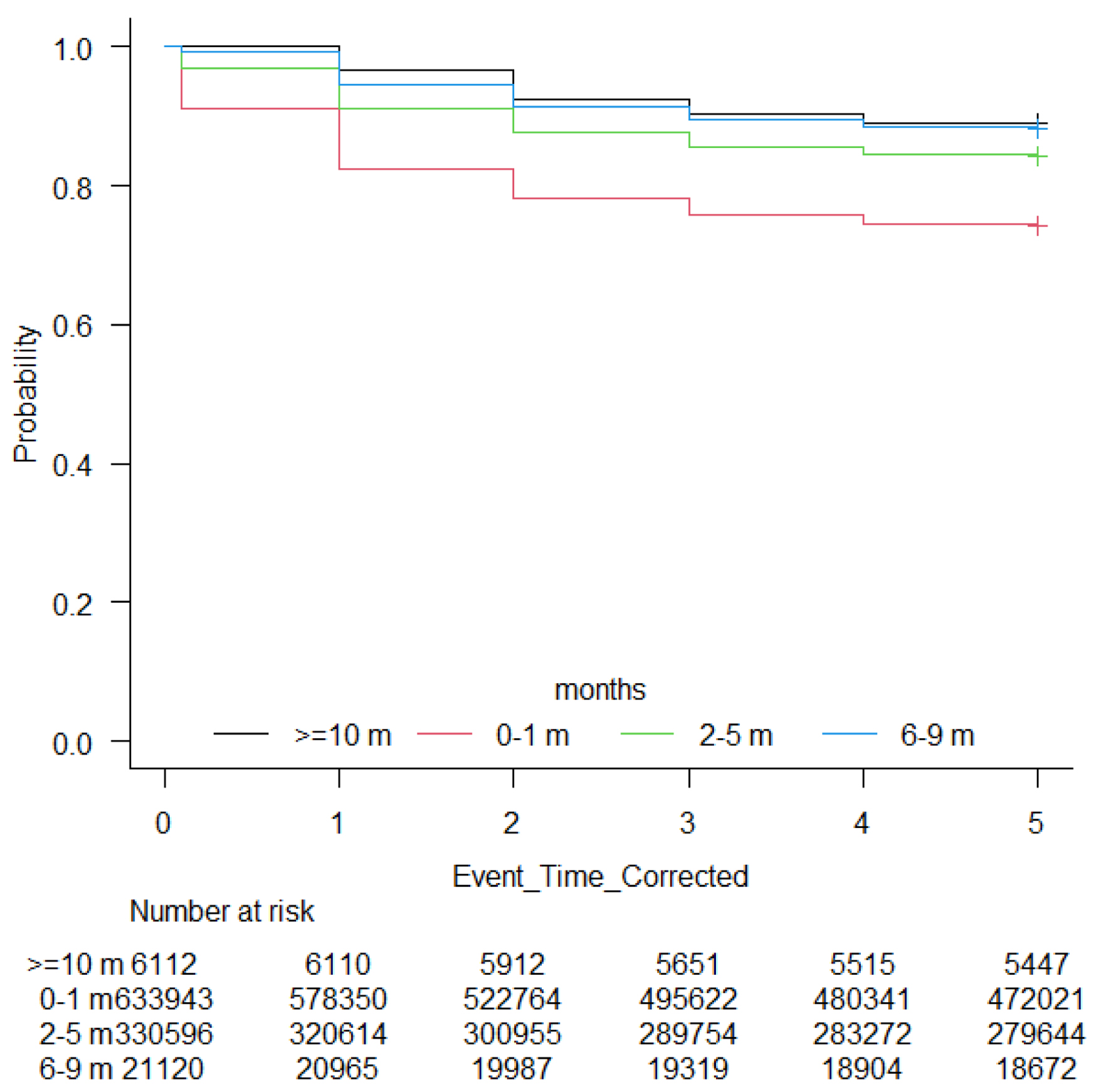
Methods: A retrospective cohort analysis was conducted using the Surveillance, Epidemiology, and End Results (SEER) database, including 991,771 adults diagnosed with breast, lung, prostate, or colorectal cancers between 2015 and 2020. TTI intervals were divided into four categories: 0 - 1, 2 - 5, 6 - 9, and ≥ 10 months. Cox proportional hazards models, adjusted for demographic, socioeconomic, cancer-specific, and treatment factors, assessed the impact of TTI on all-cause mortality, accounting for time-varying covariates.
Results: Overall, 63.9% of patients initiated treatment within 1 month. Unadjusted analyses revealed paradoxically lower mortality with longer TTI intervals (26.1% for 0 - 1 month vs. 11.4% for ≥ 10 months). After adjusting for time-varying effects, longer TTI significantly correlated with higher mortality risks (hazard ratio (HR): 1.02 for 2 - 5 months, 1.08 for 6 - 9 months, 1.23 for ≥ 10 months; P < 0.001 each), compared to treatment within 1 month. Older age (HR: 1.06), male gender (HR: 1.08), unmarried status (HR: 1.06), and non-Hispanic Black race (HR: 1.03) were independently associated with increased mortality. Lung cancer patients had significantly higher mortality than breast, prostate, and colorectal cancers (all P < 0.001). Treatment differences emerged, with reduced chemotherapy (40.2% to 10.0%) and surgical interventions (70.6% to 48.8%) at longer intervals.
Conclusion: Our analysis showed that increased TTI is independently associated with significantly higher all-cause mortality across major cancers, emphasizing the urgency of timely treatment initiation. Sociodemographic disparities in TTI and outcomes highlight systemic barriers disproportionately affecting vulnerable populations, necessitating targeted interventions to improve equitable cancer care and survival outcomes.
Published
Issue
Section
License
Copyright (c) 2025 The authors

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.