Association Between Platelet-to-Lymphocyte Ratio and Insulin Resistance in Cancer Survivors: A Cross-Sectional Study Based on the NHANES 2005 - 2018
DOI:
https://doi.org/10.14740/wjon2603Keywords:
Platelet-to-lymphocyte ratio, Insulin resistance, Cancer survivors, NHANESAbstract
Background: The incidence of insulin resistance (IR) among cancer survivors is significantly higher than that in the general population. Current diagnostic methods for IR are complex, often requiring fasting blood samples, specialized laboratory tests, and sometimes invasive procedures, which limit their routine clinical application. This study investigated the association between platelet-to-lymphocyte ratio (PLR), a readily available marker from routine blood tests, and IR in cancer survivors, aiming to find a more straightforward predictor of IR that could potentially simplify screening and monitoring processes in this high-risk population.
Methods: This cross-sectional study analyzed data from 1,418 cancer survivors from the NHANES 2005-2018 database. IR was assessed by three indicators: homeostasis model assessment of insulin resistance (HOMA-IR), quantitative insulin sensitivity check index (QUICKI), and the triglyceride-glucose (TyG) index. Multivariable logistic regression models were used to examine the relationship between PLR quartiles and IR, with restricted cubic spline (RCS) analyses to evaluate non-linear relationships. Covariates included demographic (age, gender, race/ethnicity), socioeconomic (marital status, education, family poverty income ratio), lifestyle (smoking status, alcohol consumption, sleep duration, physical activity) and health status variables (body mass index (BMI), history of cardiovascular disease, hypertension status). Subgroup analyses were conducted to identify sensitive populations.
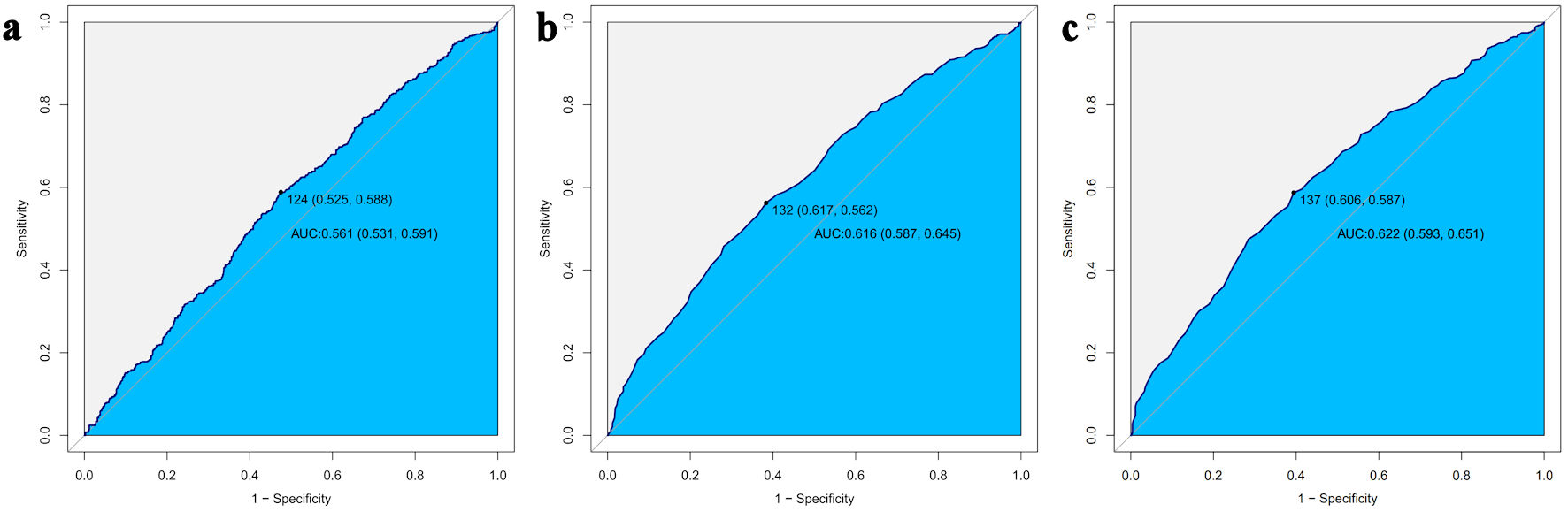
Results: The 1,418 cancer survivors (weighted population: 20,233,847; median age 69.0 years; 58.4% female) with low HOMA-IR (< 2.5), high QUICKI (≥ 0.33) and low TyG index (< 4.68) demonstrated more favorable metabolic profiles, including lower PLR values, better socioeconomic status, better lifestyle, and lower chronic disease burden. Compared to the lowest PLR quartile (Q1), individuals in the highest quartile (Q4) showed significantly increased IR risk when assessed by QUICKI (hazard ratio (HR) = 1.61, 95% confidence interval (CI): 1.02 - 2.53, P = 0.040) and the TyG index (HR = 1.56, 95% CI: 1.02 - 2.45, P = 0.035). Each increment in PLR quartile was associated with a 19% (QUICKI) and 15% (TyG) increased risk of IR. Receiver operating characteristic (ROC) analysis results indicated that PLR cutoff values in the range of 124 - 137 can serve as screening thresholds for IR in cancer survivors. In the subgroup analysis, the PLR and IR showed no significant interaction across all examined subgroup characteristics in both the HOMA-IR and QUICKI models (P > 0.05). However, in the TyG index model, individuals in the Q4 compared to the Q1 demonstrated greater susceptibility to IR in those with physical activity < 600 metabolic equivalent of task (MET)-mins/week (odds ratio (OR) = 2.28, 95% CI: 1.12 - 4.61); and those with a history of hypertension (OR = 1.95, 95% CI: 1.05 - 3.63), with P values for interaction of 0.007 and 0.036, respectively.
Conclusions: Higher PLR levels indicated a significantly increased risk of IR in cancer survivors, especially when assessed by QUICKI and the TyG index. This relationship showed no significant interaction between subgroups in the HOMA-IR and QUICKI models, but in the TyG index model, and the association was more pronounced among individuals with low physical activity and those with a history of hypertension. As a simple, cost-effective biomarker derived from routine blood tests, PLR offers potential clinical value for the assessment of IR risk in cancer survivors, especially in high-risk subgroups.
Published
Issue
Section
License
Copyright (c) 2025 The authors

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.