Proportional Frequency and Clinical Characteristics of Gastric, Esophageal, and Gastroesophageal Junction Cancers in a Private Medical Group in Brazil
DOI:
https://doi.org/10.14740/wjon2551Keywords:
Adenocarcinoma, Biomarker, Brazil, Cancer, Esophageal, Gastric, Gastroesophageal junction, Proportional frequencyAbstract
Background: Gastric cancer (GC) and esophageal cancer (EC) are among the most prevalent malignancies globally and are leading causes of cancer-related mortality. Gastroesophageal junction cancer (GEJC) is considered a distinct entity with specific histopathological characteristics. This study aimed to determine the proportional frequency of GEJC; the clinicopathological characteristics of GC, EC, and GEJC; and adherence to clinical diagnostic guidelines using data from a large private healthcare network in Brazil.
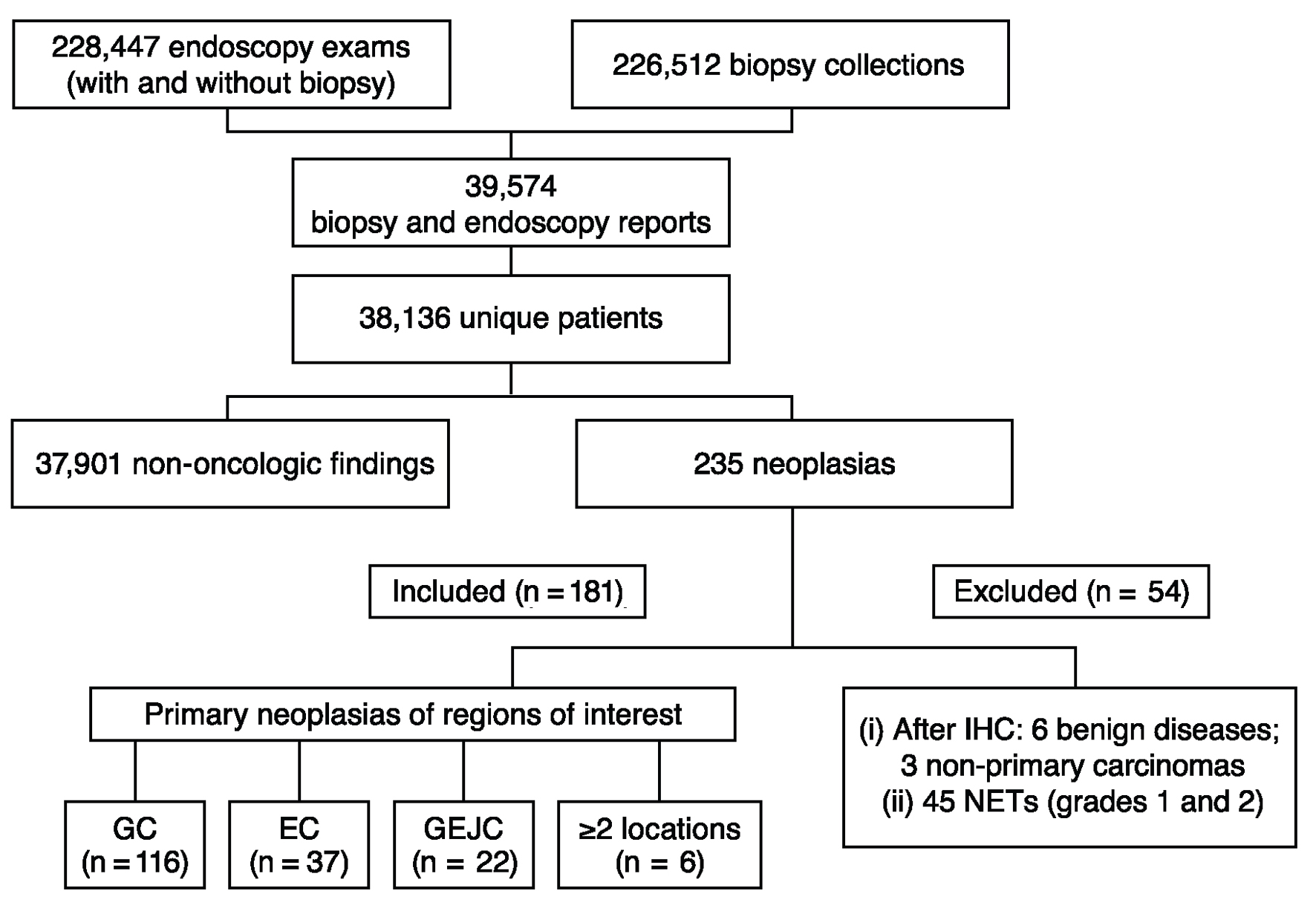
Methods: In this retrospective, cross-sectional, descriptive study and database review, records from a Brazilian medical group (Dasa) were evaluated for adults (aged ≥ 18 years) who underwent upper digestive endoscopy between July 1, 2019, and June 30, 2022. Test results from the biopsy date associated with GC, EC, or GEJC diagnosis through December 2022 were collected retrospectively.
Results: In total, 181 patients were evaluated, including 116 (64.1%) with GC, 37 (20.4%) with EC, 22 (12.2%) with GEJC, and six (3.3%) with lesions in ≥ 2 locations of interest. The ratio of GEJC to GC cases was 0.190, and the ratio of GEJC to EC cases was 0.595. Median (interquartile range) age at diagnosis was 67 (60 - 76) years, and most patients (57.5%) were aged 60 - 79 years. Sixty-two (53.4%), 27 (73.0%), 17 (77.3%), and four (66.7%) patients with GC, EC, GEJC, and lesions in ≥ 2 locations of interest, respectively, were male. The most frequently observed Lauren subtype was intestinal type for both GC and GEJC (68 (58.6%) patients and 18 (81.8%) patients, respectively). Adenocarcinoma was the most frequent histologic subtype observed in patients with EC (n = 21; 56.8%). Among patients with GC, EC, or GEJC and immunohistochemical biomarker testing, human epidermal growth factor receptor 2 expression was positive in 2/28 (7.1%), 1/3 (33.3%), and 1/2 (50.0%) patients, respectively, and mismatch repair deficiency was detected in 2/28 (7.1%), 0/3 (0%), and 0/2 (0%) patients. No patients with GEJC were tested for programmed cell death ligand 1 or claudin 18.2.
Conclusions: An improved understanding of GEJC characteristics in Brazil is essential for facilitating early diagnosis, identifying optimal treatment strategies, and informing public health policies. The extremely low rates of biomarker testing in this study revealed a significant gap in the implementation of modern oncology guidelines.
Published
Issue
Section
License
Copyright (c) 2025 The authors

This work is licensed under a Creative Commons Attribution 4.0 International License.