| World Journal of Oncology, ISSN 1920-4531 print, 1920-454X online, Open Access |
| Article copyright, the authors; Journal compilation copyright, World J Oncol and Elmer Press Inc |
| Journal website https://wjon.elmerpub.com |
Original Article
Volume 17, Number 1, February 2026, pages 52-62
Organ-Specific Clinicopathological Features That Are Associated With Post-Relapse Survival of Metastatic Breast Cancer in Japanese Women: A Multicenter Cohort Study
Yoichi Koyamaa , Yoshiya Horimotoa, b, g
, Akimitsu Yamadac
, Kazutaka Naruid
, Shinya Yamamotoe
, Hiroshi Kaisea
, Kimito Yamadaf
, Takashi Ishikawaa
aDepartment of Breast Surgical Oncology, Tokyo Medical University Hospital, Tokyo, Japan
bDepartment of Breast Oncology, Juntendo University Faculty of Medicine, Tokyo, Japan
cDepartment of Gastroenterological Surgery, Yokohama City University Graduate School of Medicine, Kanagawa, Japan
dDepartment of Breast and Thyroid Surgery, Yokohama City University Medical Centre, Kanagawa, Japan
eDepartment of Breast Surgery, Yokohama Rosai Hospital, Kanagawa, Japan
fDepartment of Breast Surgical Oncology, Tokyo Medical University Hachioji Medical Centre, Tokyo, Japan
gCorresponding Author: Yoshiya Horimoto, Department of Breast Surgical Oncology, Tokyo Medical University Hospital, Shinjuku-ku, Tokyo 160-0023, Japan
Manuscript submitted August 27, 2025, accepted October 29, 2025, published online December 17, 2025
Short title: Site-Specific Prognosis in Japanese MBC Women
doi: https://doi.org/10.14740/wjon2662
| Abstract | ▴Top |
Background: Metastatic breast cancer (MBC) presents heterogeneous clinical behavior depending on the metastatic site and molecular subtype. However, only a few studies have directly compared prognostic outcomes by the organ of initial distant recurrence. This multi-institutional retrospective study aimed to clarify the clinical and biological characteristics of MBC based on cases with single-organ metastasis at the time of initial MBC diagnosis, using real-world data from Japanese patients.
Methods: We retrospectively analyzed 309 Japanese women treated for early-stage breast cancer at six institutions between 2007 and 2021, who developed distant recurrence confined to a single organ (brain, lungs, liver, or bones) as the first site of metastasis. Patients with multi-organ metastases at initial recurrence were excluded.
Results: The median distant metastasis-free survival and post-relapse survival (PRS) were 29.4 and 39.7 months, respectively. PRS was longest in patients with bone recurrence, followed by those with lung and liver recurrence, and shortest in those with brain recurrence (P < 0.001). Bone and lung metastases were more frequently associated with hormone receptor-positive tumors, whereas liver and brain metastases were enriched for human epidermal growth factor receptor 2 (HER2)-negative and triple-negative tumors. The multivariable Cox model identified older age, triple-negative subtype, and symptomatic recurrence as independent poor prognostic factors, while liver and brain metastases were also independently associated with shorter PRS. Site-specific analyses revealed that triple-negative subtype and symptomatic presentation were consistent markers of poor prognosis across most metastatic sites.
Conclusions: Based on a single-organ metastasis cohort, this study identified distinctive clinicopathological features and survival outcomes according to the site of initial distant recurrence. Brain metastases were associated with the poorest outcomes, highlighting the need for improved risk stratification and treatment strategies.
Keywords: Breast neoplasms; Neoplasm metastasis; Molecular typing; Prognosis; Brain neoplasms; Retrospective studies
| Introduction | ▴Top |
Breast cancer is the most common cancer among women worldwide, and while its mortality has significantly decreased in high-income countries such as the United States, it has continued to increase in Japan [1]. While many patients have favorable outcomes, with 5-year relative survival rates exceeding 90% in Japanese patients [2], the development of recurrence or distant metastasis leads to a marked decrease in survival, with the 5-year survival rate for those with distant metastases dropping to around 40% [2]. Therefore, improving the prognosis of metastatic breast cancer (MBC) remains an important clinical challenge.
Among patients who develop MBC following curative treatment of primary breast cancer, common sites of metastasis include the bones, liver, lungs, and brain [3], and metastases in these organs are known to impact the behavior and prognosis of MBC. For instance, patients with bone metastasis, unaccompanied by visceral involvement, reportedly have a median overall survival of about 50 months, indicating a relatively favorable prognoses based on a French multicenter cohort study [4]. Conversely, prognoses become extremely poor once brain metastasis occurs, with median survival typically ranging from 12 to 18 months in cohorts from the United States [5]. These observations suggest that the site of distant metastasis plays a crucial role in determining clinical outcomes in MBC. However, most existing studies have analyzed cohorts that included a substantial proportion of patients with metastases to multiple organs at diagnosis. As a result, it remains difficult to isolate the prognostic implications of individual metastatic sites. A few population-based studies using the Surveillance, Epidemiology, and End Results (SEER) database in the United States have shown that patients with bone-only metastasis have the most favorable survival, while those with brain-only metastasis have the poorest outcomes [6-8]. Similarly, a nationwide Danish registry study demonstrated a similar trend [9]. Nonetheless, these studies were limited by a lack of detailed information on treatment and disease progression, and they primarily focused on Western populations. Given the possibility of racial differences in metastatic patterns and outcomes, further investigation targeting Asian cohorts, particularly Japanese patients, is warranted.
A focus on patients with single-organ metastasis at the time of initial recurrence holds several important advantages. It allows for the evaluation of the biological and prognostic characteristics specific to each metastatic site while minimizing the confounding effects of additional metastatic spread. This approach is also critical for elucidating the relationship between metastatic organ preference and tumor molecular subtypes. Furthermore, as the site of initial metastasis strongly influences therapeutic decisions, site-specific prognostic data can provide valuable support for individualized treatment planning. Such insights may also facilitate risk stratification based on organotropism and contribute to the broader understanding of metastatic mechanisms. Therefore, we aimed to use real-world data to elucidate the biological features of MBC in Japanese patients, with a particular focus on the prognostic relevance of single-organ metastasis at initial recurrence.
| Materials and Methods | ▴Top |
Patient cohorts
This was a multi-institutional, retrospective cohort study involving Japanese female patients with primary early-stage breast cancer treated at six institutions between January 2007 and December 2021. The participating institutions were Tokyo Medical University Hospital, Tokyo Medical University Hachioji Medical Center, Yokohama City University Graduate School of Medicine, Yokohama City University Medical Center, Yokohama Rosai Hospital and Juntendo University Hospital. The study design is summarized in Figure 1. Clinical data, including patient background and tumor characteristics, were retrospectively collected from medical records. For this analysis, we focused on patients who developed distant recurrence limited to a single organ - either the brain, lungs, liver, or bones - as the initial metastatic site. The following patients were excluded from this analysis: patients with disseminated carcinomatosis of the bone marrow at the time of initial bone metastasis; non-brain central nervous system involvement (such as spinal cord, pituitary gland, paranasal sinus, or leptomeningeal carcinomatosis); or pleural involvement without parenchymal lung metastasis. Patients with liver-only metastasis presenting with visceral crisis, defined according to the Advanced Breast Cancer (ABC) guidelines as rapidly increasing bilirubin levels, were also excluded [10]. After applying these criteria, a total of 309 patients were included and classified into four groups according to the site of initial distant recurrence: brain (n = 49), lungs (n = 91), liver (n = 64), and bones (n = 105). Treatment strategies before and after recurrence varied across participating institutions.
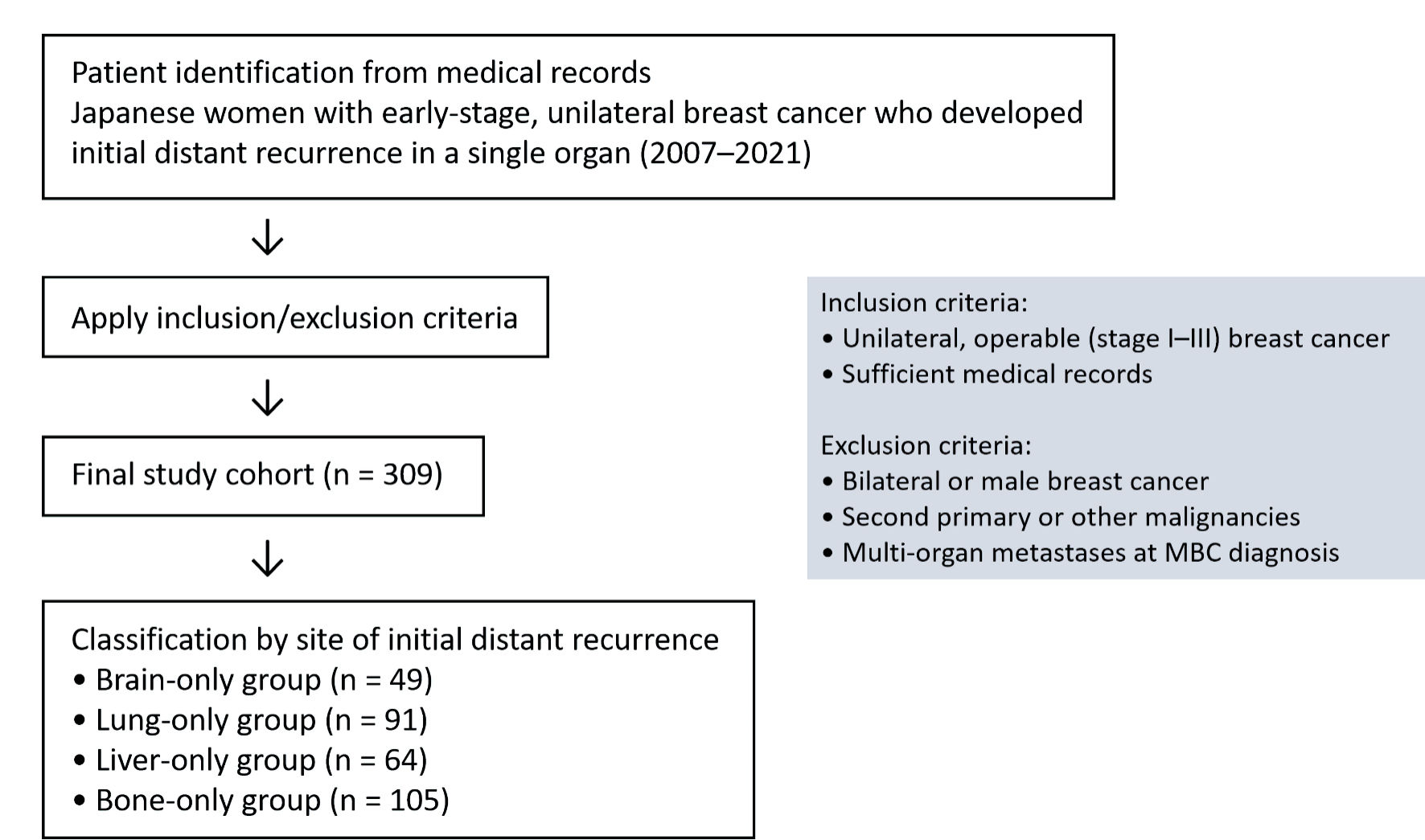 Click for large image | Figure 1. Flow diagram of study design. A flow diagram of the study design, including inclusion and exclusion criteria, is shown. MBC: metastatic breast cancer. |
Post-recurrence survival (PRS) was defined as the time from the diagnosis of MBC to death from any cause or the last follow-up. The primary objective of this study was to compare PRS according to the site of initial distant recurrence. Additionally, exploratory analyses were performed to identify clinicopathological factors associated with prognosis in each metastatic site.
This study was approved by the Ethics Committee of Tokyo Medical University (approval number: T2022-0044) and the Institutional Review Board of each participating institution. Owing to the retrospective nature of the study, the requirement for informed consent was waived. Patients could review the research plan on the hospitals’ websites and were given the option to opt out of the study at any time. This study was conducted in compliance with the ethical standards of the responsible institution on human subjects as well as with the Helsinki Declaration.
Pathological assessment
All pathological reports were retrospectively reviewed. Pathological assessments across institutions were performed uniformly based on the following criteria. Histopathological diagnosis followed the World Health Organization (WHO) classification, and tumor staging was based on the Union for International Cancer Control (UICC) TNM classification system. Nuclear grade was evaluated using the modified Bloom-Richardson system [11]. The Ki67 labeling index was assessed in a hotspot and categorized as low (≤ 20%) and high (> 20%). Estrogen receptor (ER) and progesterone receptor (PR) were considered positive when > 1% of tumor cell nuclei were stained. Human epidermal growth factor receptor 2 (HER2) was judged as positive if > 10% of the tumor cells exhibited strong staining of the entire cell membrane or if HER2/neu gene amplification was confirmed using fluorescence in situ hybridization. Molecular subtypes were classified as luminal (ER and/or PR positive, HER2 negative), luminal-HER2 (ER and/or PR positive, HER2 positive), HER2-enriched (ER and PR negative, HER2 positive), and triple-negative (ER, PR, and HER2 negative; triple-negative breast cancer (TNBC)).
Statistical analyses
All statistical analyses were conducted using the IBM SPSS Statistics, Version 29 software package (IBM Corp., Armonk, NY, USA). Continuous and categorical variables were compared between cohort groups by using Kruskal-Wallis and Pearson’s Chi-square tests, respectively. Patient follow-up was monitored until October 2023, and prognostic analysis was conducted in November 2023. Kaplan-Meier survival curves were used to estimate the median PRS (95% confidence interval (CI)), which were compared using the log-rank test. Hazard ratios (HRs) and 95% CIs for factors potentially influencing PRS were estimated using univariate and multivariable Cox proportional hazards models. For the multivariable Cox regression analysis, variables were selected based on their clinical relevance, including age, Ki67 labeling index, molecular subtype, organ of initial distant recurrence, and primary trigger for MBC diagnosis. All tests were two-tailed, and P values < 0.050 were considered indicative of statistical significance.
| Results | ▴Top |
Clinical and pathological features according to organ of initial distant recurrence organ
The clinicopathological features of the 309 patients included in this study are compared according to the site of initial distant metastasis in Table 1. The median ages at primary breast cancer and MBC diagnoses were 58 (range: 21 - 89) and 61 (range: 29 - 90) years, respectively, and there were no differences among metastatic sites. Over 80% of patients had clinical stage II or higher diseases, and nearly 70% received perioperative chemotherapy. Notably, the brain-only group had a more advanced clinical stage, whereas a significantly higher proportion of patients in this group had an earlier pathological stage compared to the other groups (P = 0.004). Among the four metastatic sites, high nuclear grade tumors were significantly less frequent in the bone-only group (P < 0.001), while the lung-only group showed a tendency toward higher Ki67 labelling index (P = 0.002). The distribution of molecular subtypes also showed a significant difference by metastatic site. The bone-only group was predominantly composed of luminal-type tumors (77%), whereas the brain-only group had a lower proportion of luminal type and a higher proportion of HER2-enriched and TNBC (P < 0.001). Regarding the timing of recurrence, the bone-only group had the longest distant metastasis-free survival (DMFS) (37 months), while the brain-only group had the shortest (14 months). Kaplan-Meier curves for DMFS according to the site of metastasis are shown here (Supplementary Material 1, wjon.elmerpub.com). As for the diagnostic triggers, the brain-only group was overwhelmingly diagnosed due to subjective symptoms such as dizziness, accounting for 96% of cases (P < 0.001). In contrast, lung and liver recurrences were most frequently detected through routine postoperative surveillance, such as imaging or tumor marker monitoring (mainly carcinoembryonic antigen (CEA) and cancer antigen 15-3 (CA15-3)). The bone-only group showed an intermediate pattern between these two. Considering the marked difference in diagnostic triggers among metastatic sites, we further calculated DMFS focusing on only patients who had subjective symptoms (n = 123; 42% of all patients) (not shown). For those patients, median DMFS were as follows: brain-only, 12.8 months (range: 1 - 154); lung-only, 14.8 (range: 6 - 61); liver-only, 21.6 (range: 6 - 134); and bone-only, 31.6 (range: 2 - 167). Although the order of median DMFS values changed slightly, the overall pattern across metastatic sites remained similar.
 Click to view | Table 1. Patients’ Clinical and Pathological Background at Baseline |
Comparison of PRS by site of initial distant metastasis and identification of prognostic factors
As of the time of this analysis, 177 patients had been confirmed to have died due to breast cancer. The median PRS for all patients was 39.7 months (95% CI: 32.3 - 47.1). First, Kaplan-Meier curves for PRS based on the organs of initial distant recurrence were drawn (Fig. 2). Patients with bone or lung metastases had the longest PRS, with median values of 48.2 months (95% CI: 37.3 - 59.1) and 47.6 months (95% CI: 33.0 - 62.2), respectively, followed by those with liver metastases at 27.4 months (95% CI: 12.5 - 42.3), whereas patients with brain metastases had the shortest PRS at 11.8 months (95% CI: 7.4 - 16.2) (P < 0.001).
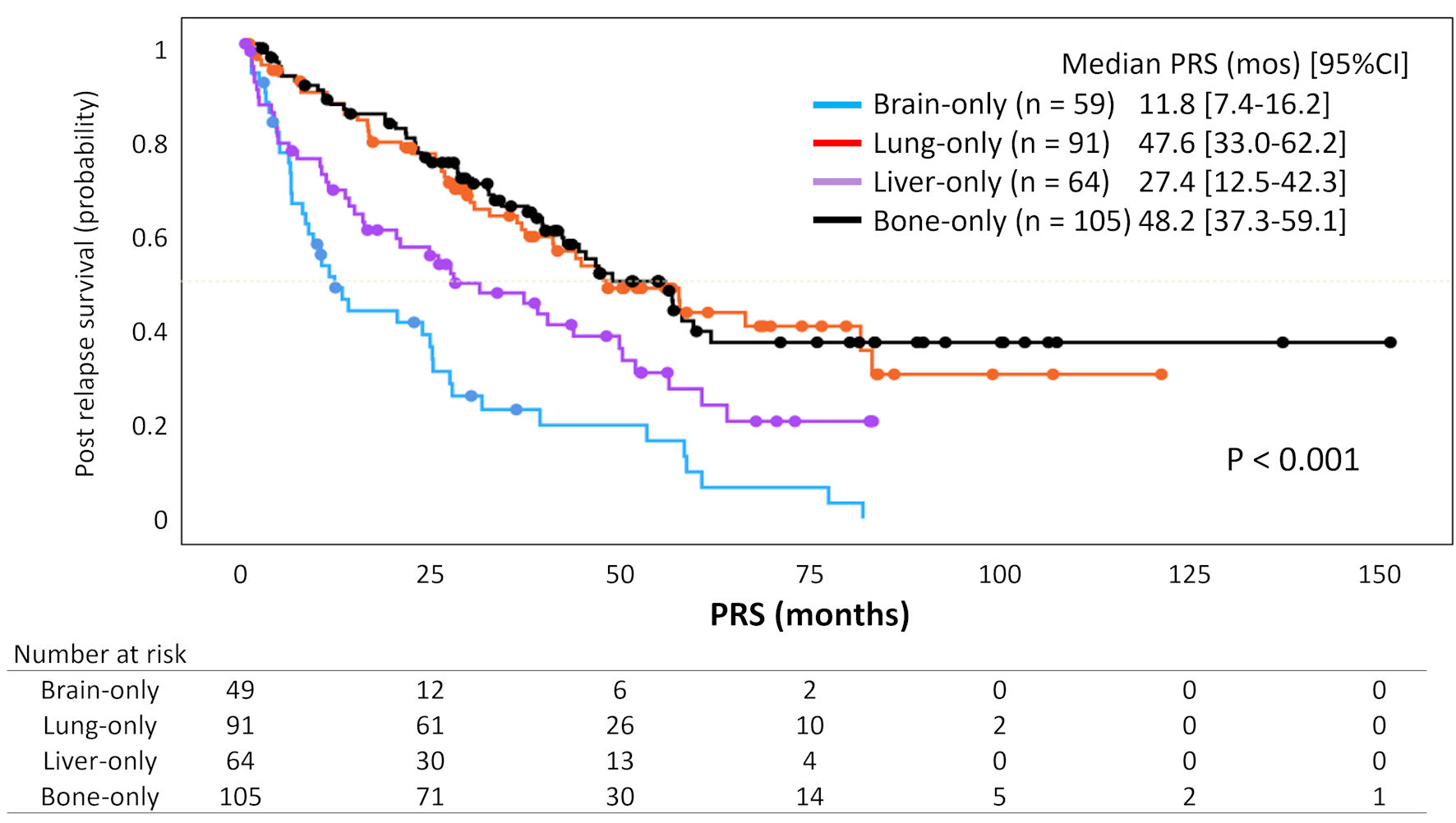 Click for large image | Figure 2. Kaplan-Meier curves for post-relapse survival according to organs of initial distant recurrence. The curves, stratified by the organs of initial distant recurrence, represent survival outcomes observed over a median follow-up period of 62.9 months (95% CI: 57.4 - 69.9). The blue, red, purple, and black curves correspond to brain-only, lung-only, liver-only, and bone-only groups, respectively. PRS: post-relapse survival; CI: confidence interval. |
Next, we investigated clinicopathological features relating to PRS. Multivariable Cox regression analysis revealed that older age at MBC diagnosis, TNBC and the presence of subjective symptoms as the primary trigger for MBC diagnosis were independent predictive factors for shorter PRS (P < 0.001, P < 0.001 and P = 0.003, respectively) (Table 2). Moreover, patients who developed brain or liver metastasis had significantly shorter PRS, compared to those with bones (median PRS: brain, 11.8 months; liver, 27.4 months; bone, 48.2 months; both P < 0.001).
 Click to view | Table 2. Factors Relating With Post-Relapse Survival (N = 309) |
Treatment patterns according to the site of initial distant recurrence
The number of drug treatment regimens administered for MBC after the diagnosis of distant recurrence is shown in Figure 3a. Among patients for whom treatment course data were available, the number of drug regimens was significantly lower in patients with brain recurrence compared to those with recurrence in other organs (P < 0.001).
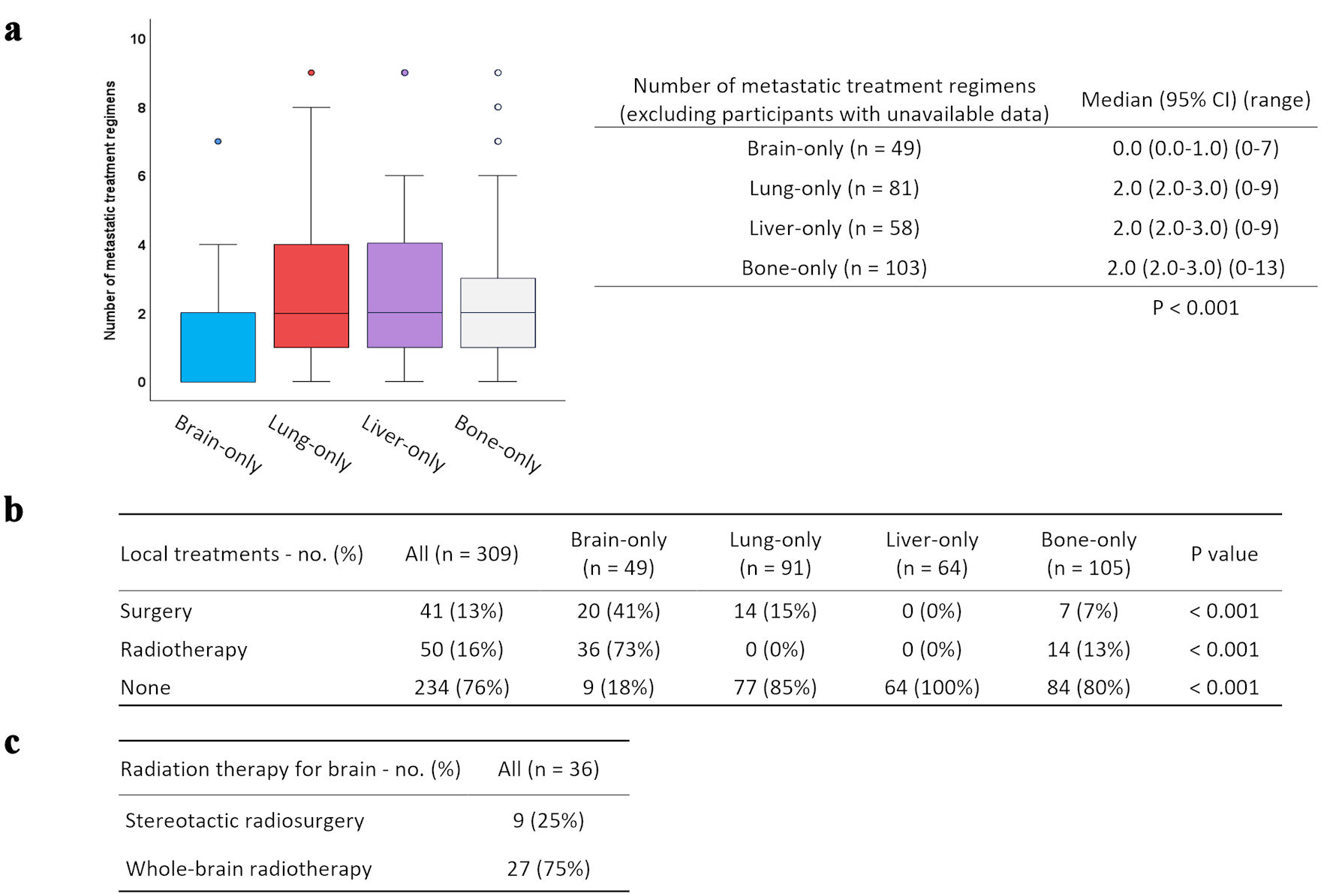 Click for large image | Figure 3. Systemic and local treatment patterns after distant recurrence according to the site of initial metastasis. (a) Number of treatment regimens for MBC according to organs of initial distant recurrence are shown and stratified by the box plots. (b) Details of local treatment for organs of initial distant recurrence. (c) Details of radiation therapy for brain metastasis. |
Next, details of the local treatment (surgery/radiotherapy) for the organs of initial distant recurrence are summarized in Figure 3b-c and were as follows. Local treatment was most frequently performed for brain metastases (82%), including surgery in 41% and radiotherapy in 73% of patients. Among the 36 patients who received radiotherapy for brain metastases, 25% underwent stereotactic radiosurgery, and 75% received whole-brain radiation therapy (WBRT), including cases in which WBRT was combined with surgical resection. For lung metastases, 15% of patients underwent surgery, all of which was performed for diagnostic purposes, and no radiotherapy was administered. No local treatment was performed for liver metastases. For bone metastases, surgery was performed in 7% and radiotherapy in 22% of patients, with all radiotherapy being delivered for palliative purposes.
Site-specific prognostic factors for PRS according to the initial distant metastasis
Given the marked differences in the primary trigger for MBC diagnosis and subsequent prognosis according to the site of metastasis, we finally performed an exploratory analysis of prognostic factors stratified by the site of initial distant metastasis. As shown in Table 3, in the brain-only group, which exhibited the poorest prognosis, patients with high nuclear grade tumors tended to have shorter PRS (P = 0.064). As for molecular subtype, when luminal tumors were used as the reference, TNBC exhibited a higher HR of 1.87 (P = 0.126), although this difference did not reach statistical significance. However, when TNBC was used as the reference, the HRs for the other subtypes were as follows; luminal (HR = 0.53, P = 0.126), luminal-HER2 (HR = 0.37, P = 0.044) and HER2-enriched (HR = 0.44, P = 0.058). Among these, luminal-HER2 tumors showed a significantly longer PRS compared to TNBC. In addition, patients who did not receive local treatment for brain metastasis also tended to have shorter PRS (P = 0.057).
 Click to view | Table 3. Site-Specific Factors Relating With Post-Relapse Survival |
In the lung-only group, shorter PRS was observed among older patients and those with high nuclear grade tumors, TNBC, or symptomatic presentation at the time of diagnosis of metastasis (P = 0.033, P = 0.011, P < 0.001, and P < 0.001, respectively). Interestingly, patients who underwent local surgery had significantly better PRS (P = 0.039); however, all surgical procedures were performed for diagnostic purposes only. Among patients who developed liver metastasis, those with TNBC or who presented with symptoms caused by liver dysfunction had significantly worse PRS (P = 0.004 and P = 0.002, respectively). Finally, in the bone-only group, patients with special histological types or TNBC had significantly worse prognosis (P = 0.010 and P = 0.018, respectively). In addition, patients who required local treatment for symptomatic bone lesions at the time of diagnosis also had significantly shorter PRS (P = 0.011).
Lastly, we compared PRS by subtype within each metastatic organ, where molecular subtype was consistently associated with prognosis, using the Kaplan-Meier curve method. As shown in Figure 4, TNBC was consistently associated with the shortest PRS across all metastatic sites. In the lung-only and liver-only groups, significant differences were observed in the distribution of Kaplan-Meier curves, reflecting the markedly worse prognosis of TNBC compared to the more favorable outcomes in the luminal type (median PRS: lung-only group, TNBC 25.8 months vs. luminal 65.6 months; liver-only group, TNBC 4.3 months vs. luminal 38.4 months; P < 0.001 and P = 0.007, respectively).
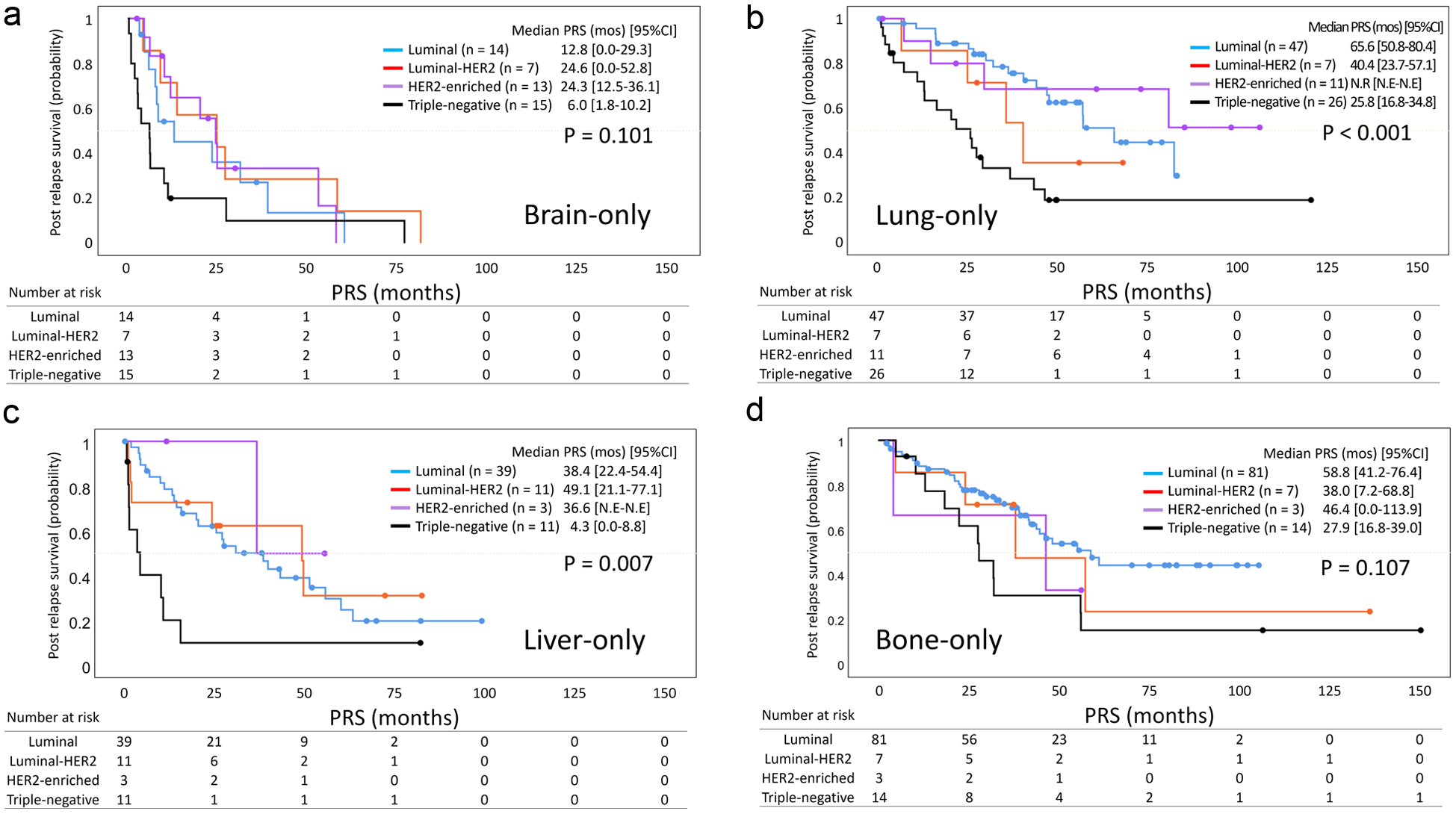 Click for large image | Figure 4. Kaplan-Meier curves of post-relapse survival by molecular subtype in each metastatic site. Kaplan-Meier curves of PRS according to molecular subtype in the (a) brain-only, (b) lung-only, (c) liver-only, and (d) bone-only groups are shown. The blue, red, purple, and black curves correspond to patients with luminal, luminal-HER2, HER2-enriched, and triple-negative MBC, respectively. Dots on each curve indicate censored cases. PRS: post-relapse survival; CI: confidence interval; N.R: not reached; N.E: not estimable; MBC: metastatic breast cancer; HER2: human epidermal growth factor receptor 2. |
| Discussion | ▴Top |
In the present study, a comparison across metastatic organs revealed several distinct features. Patients with HER2-enriched tumors had a higher propensity for brain metastasis, those with TNBC more frequently developed brain and lung metastases, and bone metastasis was most commonly observed in patients with luminal-type tumors. This trend is consistent with findings from previous clinical and preclinical studies [12-14]. Moreover, DMFS varied significantly depending on the metastatic site, with a trend indicating that the timing of recurrence differed among organs: longest for bone, followed by lung, and shortest for brain.
Several previous studies have reported that patients with bone-only metastases have more favorable survival outcomes compared to those with lung-only metastasis [8, 15, 16]. Meanwhile, some reports have suggested that the prognostic difference between bone and lung metastases may be minimal, with survival curves for the two sites being relatively close [6, 7]. In the present study as well, no significant difference in PRS was observed between the bone-only and lung-only groups. This result may be partly explained by the possibility that a relatively large proportion of lung metastases were detected through routine follow-up examinations without any symptom. In addition, some lung lesions required surgical confirmation because of their small or solitary nature, which may have been associated with better prognosis in these patients. Alternatively, recent advances in systemic therapy for recurrent breast cancer may have contributed to improved prognosis in patients with lung metastases. Nevertheless, the difference in prognosis between these two groups may not be substantial. Some population-based studies have shown site-specific survival differences in single-organ metastasis, but the prognostic gap between bone-only and lung-only disease remains unclear, consistent with our finding of comparable outcomes [8, 9].
Prognostic factors associated with PRS were also explored for each metastatic organ, revealing distinct patterns in each group. TNBC was a common poor prognostic factor across all metastatic sites. In the brain metastasis group, high nuclear grade and absence of local treatment tended to be associated with worse prognosis. In the lung metastasis group, advanced age and symptom-driven diagnosis were linked to shorter PRS. In the liver group, symptomatic recurrence accompanied by hepatic dysfunction was a poor prognostic indicator, while in the bone group, tumors with special histological types and symptomatic lesions requiring local treatment were associated with unfavorable outcomes. A notable finding was that the presence of symptoms at the time of diagnosis varied across metastatic sites and was associated with prognosis. While nearly all patients with brain metastases were diagnosed based on neurological symptoms, the presence of symptoms was statistically associated with shorter PRS in both the lung-only and liver-only groups. In the bone-only group as well, poor outcomes were observed in patients who presented with advanced symptoms severe enough to require local intervention, such as pain or pathological fractures. These findings may reflect that symptomatic recurrence is often associated with more advanced metastatic disease and impaired performance status, both of which contribute to poor prognosis. As for the brain-only group, 96% of patients were diagnosed after the onset of neurological symptoms, indicating that asymptomatic detection was extremely rare and that brain metastases were often identified at an advanced stage, potentially limiting subsequent treatment options. This may also explain why local treatment could not be applied in some patients with brain metastases. Meanwhile, recent agents such as trastuzumab deruxtecan (T-DXd) have demonstrated intracranial efficacy [17-19], and their benefits may be greater if treatment is initiated earlier. Therefore, developing strategies to detect brain metastases during the asymptomatic phase, through improved risk stratification or predictive markers, may be important. Based on our findings, clinical features such as advanced initial stage, TNBC or HER2-enriched subtype, and favorable response to neoadjuvant therapy (e.g., pathological complete response), which was observed in a relatively high proportion of patients with brain metastasis in our cohort, may help identify a subset of patients who are at risk of early distant recurrence such as brain metastasis, despite favorable initial response. Additionally, noninvasive methods such as liquid biopsy may offer promising tools for early detection in the future.
Major limitations in the current study include its retrospective design based on real-world data, which raises concerns about potential selection bias across metastatic site groups. This bias may arise from differences in the detectability of metastases depending on postoperative surveillance strategies. For instance, metastases to organs such as the lungs or liver are more likely to be detected through routine imaging or laboratory monitoring, whereas brain metastases are often identified only after the onset of symptoms. In addition, the methods of postoperative surveillance and treatment strategies for MBC may have varied, as follow-up schedules were determined by each physician’s discretion, reflecting real-world clinical practice in Japan. Second, this study focused on patients with initial distant recurrence limited to a single organ and excluded those with multi-organ metastases. However, information to determine whether these lesions represented true oligometastatic disease was unavailable, which prevented a more detailed evaluation of its prognostic implications. Another limitation is that aggressive special forms of metastasis regarded as rapidly progressive variants within each organ, such as liver crisis in liver metastasis, were excluded from this analysis. Although this exclusion aimed to ensure comparability of disease burden across metastatic sites, it may have resulted in the underrepresentation of highly aggressive disease phenotypes. Furthermore, for the included patients, detailed information on post-recurrence disease progression or additional organ metastases could not be obtained. Such information would be important for evaluating whether the prognosis is determined mainly by the initial metastatic site or by subsequent disease evolution, as demonstrated in previous large-scale studies [8, 20]. Future prospective studies with longitudinal follow-up are warranted to address this issue.
Nevertheless, to the best of our knowledge, no other large-scale studies have focused specifically on the biology of MBC in Asian populations, examining initial distant recurrence to single, anatomically distinct organs. A key strength of this study lies in its strict inclusion of patients with single-organ metastasis, which enabled a focused comparison of the biological characteristics and clinical features associated with metastasis to each organ. Previous studies investigating single-organ metastasis have mostly been conducted in Western populations, whereas our results, derived from a Japanese cohort, generally aligned with these findings. This suggests that the prognostic impact of metastatic organ site may be broadly consistent across different ethnic and healthcare settings.
Conclusions
Based on a single-organ metastasis cohort, this study demonstrated that MBC exhibits distinct prognostic patterns depending on the site of initial distant recurrence. Particularly, brain metastasis was associated with markedly poor outcomes, likely due to advanced disease status at diagnosis and limited therapeutic options. These findings may serve as a foundation for future efforts in risk stratification and treatment planning for recurrent breast cancer.
| Supplementary Material | ▴Top |
Suppl 1. Kaplan-Meier curves for distant metastasis-free survival according to the site of initial distant metastasis.
Acknowledgments
None to declare.
Financial Disclosure
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflict of Interest
The authors declare no conflict of interest to disclose.
Informed Consent
Owing to the retrospective nature of the study, the requirement for informed consent was waived. Patients could review the research plan on the hospitals’ websites and were given the option to opt out of the study at any time.
Author Contributions
YK and TI contributed to the study’s conception and design. YK, YH, AY, KN, SY, and KY collected clinical data. YK and YH conducted data analysis and statistics. YK and YH drafted the original manuscript, and AY, KN, SY, HK, KY and TI substantively revised it. All authors have read and approved the manuscript.
Data Availability
All data supporting the findings of this study are available within the paper and its supplementary material.
Abbreviations
ABC: advanced breast cancer; CI: confidence interval; DMFS: distant metastasis-free survival; ER: estrogen receptor; HER2: human epidermal growth factor receptor 2; MBC: metastatic breast cancer; PR: progesterone receptor; PRS: post-relapse survival; SEER: Surveillance, Epidemiology, and End Results; T-DXd: trastuzumab deruxtecan; TNBC: triple-negative breast cancer; WBRT: whole-brain radiation therapy
| References | ▴Top |
- Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, Bray F. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71(3):209-249.
doi pubmed - Ito Y, Miyashiro I, Ito H, Hosono S, Chihara D, Nakata-Yamada K, Nakayama M, et al. Long-term survival and conditional survival of cancer patients in Japan using population-based cancer registry data. Cancer Sci. 2014;105(11):1480-1486.
doi pubmed - Largillier R, Ferrero JM, Doyen J, Barriere J, Namer M, Mari V, Courdi A, et al. Prognostic factors in 1,038 women with metastatic breast cancer. Ann Oncol. 2008;19(12):2012-2019.
doi pubmed - Xiong Z, Deng G, Huang X, Li X, Xie X, Wang J, Shuang Z, et al. Bone metastasis pattern in initial metastatic breast cancer: a population-based study. Cancer Manag Res. 2018;10:287-295.
doi pubmed - Puri S, Chaudhry A, Bayable A, Ganesh A, Daher A, Gadi VK, Maraka S. Systemic treatment for brain metastasis and leptomeningeal disease in breast cancer patients. Curr Oncol Rep. 2023;25(12):1419-1430.
doi pubmed - Chen MT, Sun HF, Zhao Y, Fu WY, Yang LP, Gao SP, Li LD, et al. Comparison of patterns and prognosis among distant metastatic breast cancer patients by age groups: a SEER population-based analysis. Sci Rep. 2017;7(1):9254.
doi pubmed - Wang R, Zhu Y, Liu X, Liao X, He J, Niu L. The Clinicopathological features and survival outcomes of patients with different metastatic sites in stage IV breast cancer. BMC Cancer. 2019;19(1):1091.
doi pubmed - Taskindoust M, Thomas SM, Sammons SL, Fayanju OM, DiLalla G, Hwang ES, Plichta JK. Survival outcomes among patients with metastatic breast cancer: review of 47,000 patients. Ann Surg Oncol. 2021;28(12):7441-7449.
doi pubmed - Ording AG, Heide-Jorgensen U, Christiansen CF, Norgaard M, Acquavella J, Sorensen HT. Site of metastasis and breast cancer mortality: a Danish nationwide registry-based cohort study. Clin Exp Metastasis. 2017;34(1):93-101.
doi pubmed - Cardoso F, Paluch-Shimon S, Schumacher-Wulf E, Matos L, Gelmon K, Aapro MS, Bajpai J, et al. 6th and 7th International consensus guidelines for the management of advanced breast cancer (ABC guidelines 6 and 7). Breast. 2024;76:103756.
doi pubmed - Robbins P, Pinder S, de Klerk N, Dawkins H, Harvey J, Sterrett G, Ellis I, et al. Histological grading of breast carcinomas: a study of interobserver agreement. Hum Pathol. 1995;26(8):873-879.
doi pubmed - Kennecke H, Yerushalmi R, Woods R, Cheang MC, Voduc D, Speers CH, Nielsen TO, et al. Metastatic behavior of breast cancer subtypes. J Clin Oncol. 2010;28(20):3271-3277.
doi pubmed - Minn AJ, Gupta GP, Siegel PM, Bos PD, Shu W, Giri DD, Viale A, et al. Genes that mediate breast cancer metastasis to lung. Nature. 2005;436(7050):518-524.
doi pubmed - Hess KR, Pusztai L, Buzdar AU, Hortobagyi GN. Estrogen receptors and distinct patterns of breast cancer relapse. Breast Cancer Res Treat. 2003;78(1):105-118.
doi pubmed - Kast K, Link T, Friedrich K, Petzold A, Niedostatek A, Schoffer O, Werner C, et al. Impact of breast cancer subtypes and patterns of metastasis on outcome. Breast Cancer Res Treat. 2015;150(3):621-629.
doi pubmed - Xie Y, Ma J, Xia X, Zheng H, Gou Q. Prognosis and treatment of metastatic breast cancer from a Real-World Scenario in China: a retrospective cohort study. Cancer Control. 2022;29:10732748221130568.
doi pubmed - Lin NU, Murthy RK, Abramson V, Anders C, Bachelot T, Bedard PL, Borges V, et al. Tucatinib vs placebo, both in combination with trastuzumab and capecitabine, for previously treated ERBB2 (HER2)-positive metastatic breast cancer in patients with brain metastases: updated exploratory analysis of the HER2CLIMB randomized clinical trial. JAMA Oncol. 2023;9(2):197-205.
doi pubmed - Cortes J, Kim SB, Chung WP, Im SA, Park YH, Hegg R, Kim MH, et al. Trastuzumab Deruxtecan versus Trastuzumab Emtansine for breast cancer. N Engl J Med. 2022;386(12):1143-1154.
doi pubmed - Modi S. Trastuzumab deruxtecan in previously treated HER2-low advanced breast cancer: a plain language summary of the DESTINY-Breast04 study. Future Oncol. 2025;21(4):367-380.
doi pubmed - Zhang M, Deng H, Hu R, Chen F, Dong S, Zhang S, Guo W, et al. Patterns and prognostic implications of distant metastasis in breast Cancer based on SEER population data. Sci Rep. 2025;15(1):26717.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (CC BY 4.0), which permits unrestricted use, distribution, and reproduction in any medium, including commercial use, provided the original work is properly cited.
World Journal of Oncology is published by Elmer Press Inc.