| World Journal of Oncology, ISSN 1920-4531 print, 1920-454X online, Open Access |
| Article copyright, the authors; Journal compilation copyright, World J Oncol and Elmer Press Inc |
| Journal website https://wjon.elmerpub.com |
Original Article
Volume 16, Number 1, February 2025, pages 113-119
Survival Analysis of Anaplastic Thyroid Carcinoma With Various Therapeutic Modalities: Twenty-Seven Years’ Experience in a Single Cancer Center
Putu Anda Tusta Adiputraa, c , I Gede Budhi Setiawana
, I Putu Gede Septiawan Saputrab
, I Wayan Sudarsaa
aDivision of Surgical Oncology, Department of Surgery, Faculty of Medicine, Udayana University, Bali, Indonesia
bFaculty of Medicine, Udayana University, Bali, Indonesia
cCorresponding Author: Putu Anda Tusta Adiputra, Division of Surgical Oncology, Department of Surgery, Faculty of Medicine, Udayana University, Bali, Indonesia
Manuscript submitted October 14, 2024, accepted December 2, 2024, published online December 31, 2024
Short title: Survival of Anaplastic Thyroid Carcinoma
doi: https://doi.org/10.14740/wjon1988
| Abstract | ▴Top |
Background: Anaplastic thyroid carcinoma (ATC) is the most aggressive thyroid gland malignancy. Several consensuses support the concept of multimodal therapy that combines surgery, radiation, chemotherapy, and targeted therapy. However, patient’s comorbidity, poor performance status, and metastasis often make it impossible for patients to undergo multimodal therapy. Therefore, this study aimed to evaluate the survival analysis of ATC patients with different therapeutic modalities.
Methods: This study was a retrospective cohort study using data from the Cancer Registry in our institution. All patients with ATC who visited Prof Ngoerah Hospital between 1998 and 2024 were included in this study. Data regarding the survival duration of patients who received treatment modalities, and clinical data were analyzed using SPSS 20.0 with Kaplan-Meier and log-rank tests.
Results: Forty-two subjects with ATC were included in the analysis, of which 57.1% were female, with a mean age of 62.57 ± 13.42 years old. The median survival is 27.5 days. This study found no association between survival time and clinical characteristics of the patients (P > 0.05). This study found that patients who received combination therapy such as surgery + chemotherapy/radiotherapy (RT) had a longer survival time (64 days), compared to other patients who received surgery only (26 days), chemotherapy/RT only (49 days), or patients who died before receiving any therapy (19 days). However, the log-rank test showed that it was not statistically different (P > 0.05).
Conclusion: ATC survival rates have remained low, and aggressive strategies are still needed to improve the prognosis.
Keywords: Anaplastic thyroid carcinoma; Survival; Therapeutic modalities
| Introduction | ▴Top |
Anaplastic thyroid carcinoma (ATC) is one of the most aggressive thyroid cancers with low survival, regardless of any therapeutic modalities [1]. ATC had a very aggressive behavior with rapidly enlarging local mass growth and distant spread [2]. The therapeutic modalities for ATC were surgery, radiotherapy (RT), chemotherapy, or targeted therapy as B-rapidly accelerated fibrosarcoma/mitogen-activated protein kinase (BRAF/MEK) inhibitor. The American Thyroid Association (ATA) recommended surgical resection for patients with confined stage (IVA/IVB) since it offers longer overall survival (OS) compared to chemotherapy and/or RT. Meanwhile, patients with unresectable disease at diagnosis may be advised of an RT approach and/or systemic therapy (chemotherapy or BRAF/MEK inhibitors) [3].
Although the survival rate of ATC patients has not improved much in the last six decades, some consensus supports the concept of multimodal therapy that combines surgery, RT, chemotherapy, and targeted therapy [4]. Previous studies showed that multimodal therapy gives a better insight into longer survival [5-7]. However, ATC patients come with advanced-stage or even metastatic conditions which causes the choice of therapy that can be given to be limited. Comorbid factors and patient performance status also often make it impossible for patients to undergo multimodal therapy [8].
This condition causes the prognosis of ATC patients to be poor with a low survival rate. Differences in the availability of health facilities, especially in low-to-middle-income countries (LMIC) also cause limited therapeutic options for ATC patients. Therefore, this study aimed to conduct the survival analysis of ATC patients with various therapeutic modalities for 27 years in a single cancer center.
| Materials and Methods | ▴Top |
Study design and patient selection
This was a retrospective cohort study sourced from the Cancer Registry in Bali, Indonesia. The inclusion criteria in this study were all patients with a diagnosis of ATC who underwent treatment at Prof Ngoerah Hospital during the period 1998 - 2024. The diagnosis of ATC was established based on the results of histopathological examination of biopsy specimens performed by a pathologist. Incomplete data were excluded from this study.
Institutional review board approval and ethical compliance
This study has received ethical clearance from The Research Ethics Committee Faculty of Medicine Udayana University with number 2381/UN14.2.2.VII.14/LT/2024. This study was conducted in compliance with the ethical standards of the responsible institution on human subjects as well as with the Helsinki Declaration.
Therapeutic modalities
Therapeutic modalities used in this study included surgery, chemotherapy, RT, or a combination of them. The selection of therapeutic modalities for each patient was based on the patient’s age, tumor size (resectable/non-resectable), performance status, distant metastasis, comorbidity, or presence of airway obstruction. The surgery options included partial (isthmectomy and isthmolobectomy) or total thyroidectomy. Tracheostomy was done in patients with impending airway obstruction, in conjunction with other surgery approaches or tracheostomy only. The chemotherapy regimen given to the patients in this study was either doxorubicin or paclitaxel-based chemotherapy. RT was given at 50 - 70 Gy in 20 - 35 fractions.
Data collection
Data collected in this study included clinicopathological data such as age at diagnosis, gender, stage, location of metastasis, Karnofsky performance score, type of therapy received, and patient clinical outcomes. The data were obtained from medical records and the cancer registry. This study followed the American Joint Committee on Cancer (AJCC) fifth-eighth edition to categorize the stage of the patients. The survival time is defined as the duration between the first time when patients were diagnosed with ATC until the patients had died.
Statistical analysis
The collected data were then analyzed using SPSS ver. 20 using non-parametric Mann-Whitney analysis and survival analysis using Kaplan-Meier and log-rank test. The results were considered significant if P < 0.05.
| Results | ▴Top |
This study successfully collected 66 samples of ATC patients treated at Prof Ngoerah Hospital during the period 1998 - 2024. The trend of ATC cases is shown in Figure 1. The number of ATC cases per year is fluctuating and there is an uptrend in the last decade. Unfortunately, due to incomplete data, a total of 24 cases were not included for further statistical analysis.
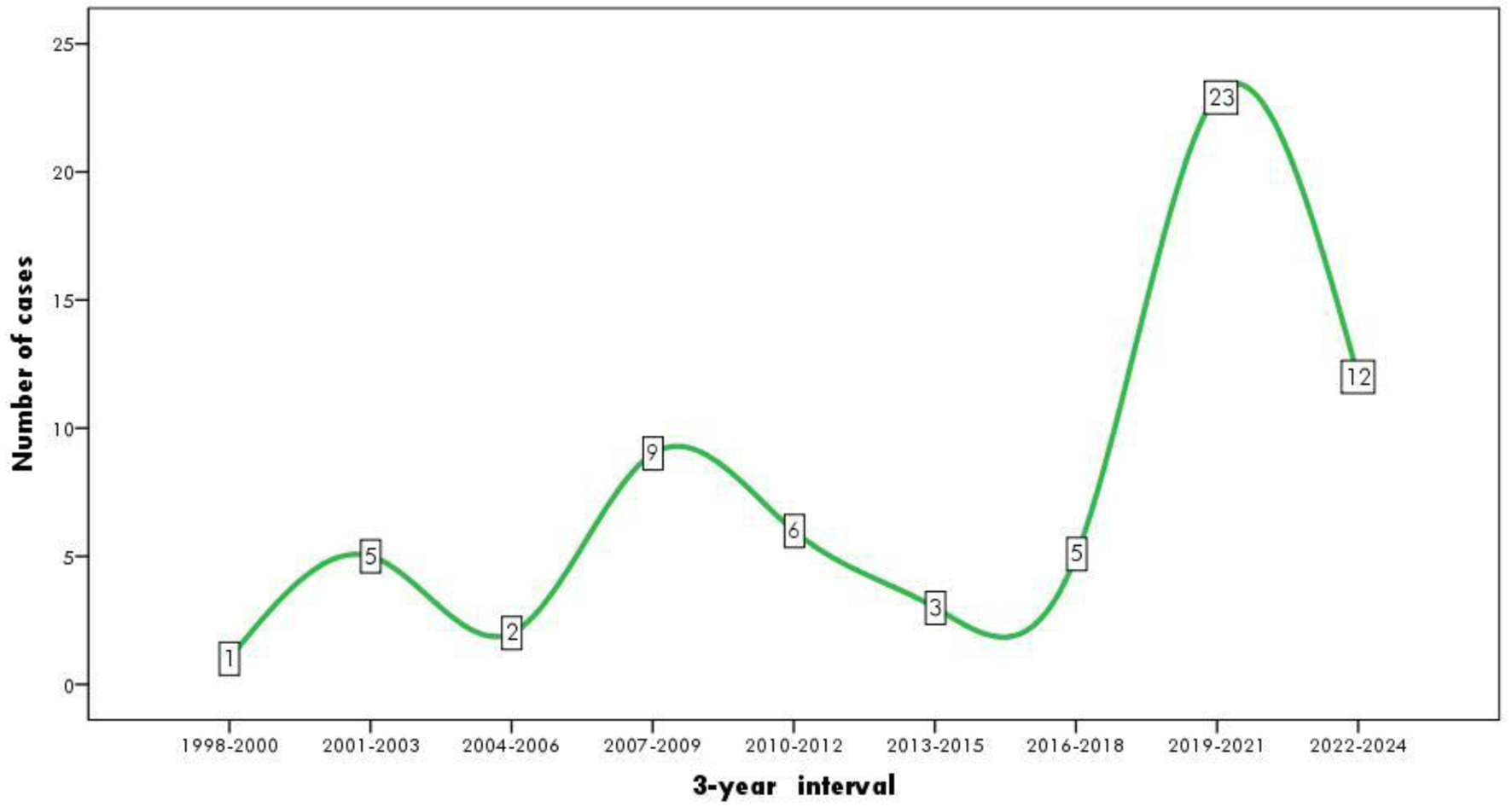 Click for large image | Figure 1. The trend of ATC cases during 1998 - 2024. ATC: anaplastic thyroid carcinoma. |
A total of 42 cases were included in the statistical analysis. This study found that the average age of patients was 62.57 ± 13.42 years, and 57.1% of the patients were female. Based on clinical conditions, stages T4a (57.1%), N1 (40.5%), and M0 (61.9%) were most commonly found in patients in this study. Most patients were found with stage IVc (40.5%), with the most metastatic locations being found in the lungs (82.3%), and as much as 64.3% of the patients had Karnofsky performance score ≤ 80 (Table 1).
 Click to view | Table 1. Baseline Characteristics of the Samples |
The median survival of patients in this study was 27.5 days. Only five (11.9%) patients received a combination of surgery and chemotherapy/RT. The most common surgical therapy option in this study was isthmectomy + tracheostomy (26.9%). Other surgical options found in this study included isthmolobectomy (23.1%), total thyroidectomy (19.2%), isthmectomy (3.8%), tracheostomy only (19.2%), and total thyroidectomy + tracheostomy (7.8%). A total of five (11.9%) patients received RT or chemotherapy only. While a total of 11 patients (26.2%) had died without receiving any therapy in this study (Table 1). This is due to the patient’s very poor condition when first arrived, so it is not possible to continue the treatment plan.
Non-parametric analysis using the Mann-Whitney U test was used to evaluate the relationship between survival and clinical characteristics of ATC patients. Young patients (≤ 60 years) had better survival time compared to patients aged > 60 years (44.63 ± 32.83 vs. 38.76 ± 31.07 days) although not significantly different (P = 0.567). Male patients had longer survival compared to female patients (48.11 ± 35.71 vs. 35.52 ± 27.30 days) although not significantly different (P = 0.208). Uniquely, this study found that patients with T4b status (42.28 ± 26.13 vs. 40.09 ± 35.69 days) had longer survival times compared to T4a patients although not statistically significant (P = 0.828). Patients with N0 and M0 in this study had longer survival compared to patients with N+ (52.06 ± 37.13 vs. 34.00 ± 25.67 days) and M1 (42.23 ± 34.76 vs. 39.00 ± 25.87 days) although not statistically significant (P = 0.073 and 0.756). Patients with stage IVc had a shorter survival time compared to patients with stage IVa/IVb (35.18 ± 26.23 vs. 45.21 ± 34.68 days) although it was not statistically different (P = 0.321). Patients with poor performance status (Karnofsky score ≤ 80) had shorter mean survival compared to patients with better performance status (Karnofsky score > 80) (37.59 ± 33.60 vs. 57.33 ± 53.47 days) but not statistically different (P = 0.149) (Table 2).
 Click to view | Table 2. Survival Time Based on Patient Clinical Characteristics |
The patients were then divided, based on their achieved treatments, into three groups. The Kaplan-Meier analysis (Fig. 2) shows that patients with combination therapy including surgery + chemotherapy or RT had longer median survival (64 days), compared to the patients who only had chemotherapy/RT (49 days) or surgery only (26 days), or patients who died before receiving any therapy (19 days). Even though, this result was not statistically different based on the log-rank test (P = 0.457) (Table 3).
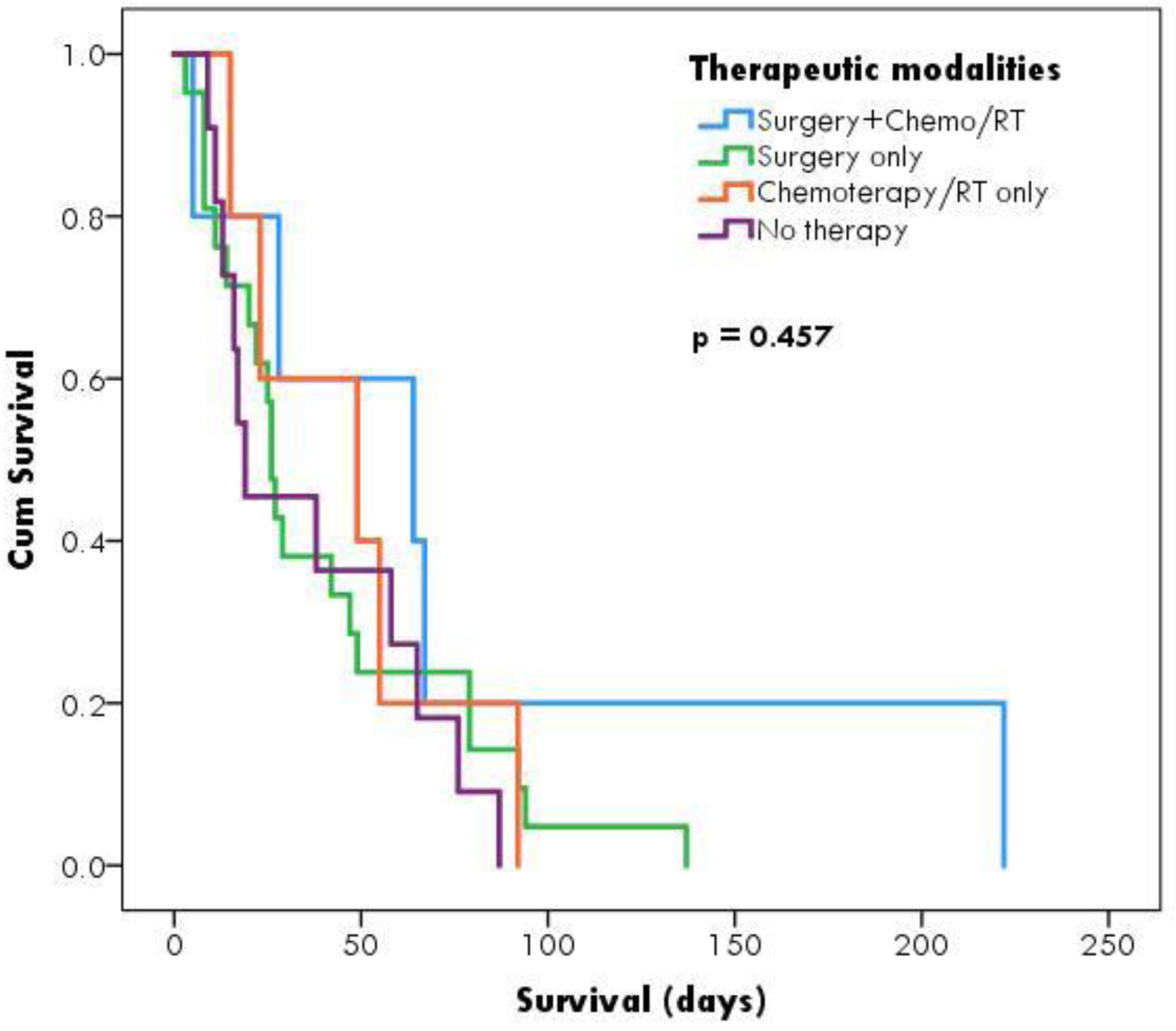 Click for large image | Figure 2. Kaplan-Meier survival analysis based on therapeutic modalities. |
 Click to view | Table 3. Survival Analysis Based on Therapeutic Modalities |
| Discussion | ▴Top |
ATC only accounted for the least common thyroid cancer subtype, but the rate of mortality was the highest [9]. Worldwide the trend incidence of ATC fluctuated, where there was a decline of cases in 1970 - 1980, but since that, it increased slightly again [10, 11]. This study found that the average age of ATC patients was > 60 years and there were more female than male patients. This finding is in accordance with the findings of several previous studies showing that ATC patients are more likely to be over 60 years old [12], and present a female predominance (female/male ratio 5.2:1) [11]. Epidemiologically, ATC occurs more in the elderly, especially in the seventh and eighth decades. The prognosis of younger ATC patients is generally better than that of older patients [13], which was also found in this study. Similar results were also found in the study by Kong et al, which found that patients aged > 70 years had a 1.6-fold shorter survival risk than patients aged < 70 years [12].
ATC patients generally have advanced-stage conditions, with the most common stage at diagnosis being IVb (35%) and IVc (55%) [11], which was also found in this study. Clinical symptoms of ATC were aggressive with a rapidly growing neck mass, the presence of neck lymph node enlargement, and/or distant metastasis. This study found that 38.1% of patients were found to be positive for metastasis at the initial diagnosis. This is in accordance with the theory that half of the diagnosed cases presented with metastases, mostly to the lungs and bone [14]. The most common metastasis site of ATC is lung (80%) [15], which was also found in this study (82.3%).
Most studies showed that ATC had a median survival of 5 - 6 months with a 1-year survival rate below 20% [16]. It was higher than this study’s findings that the median survival of the patients was only 27.50 days after being diagnosed with ATC. This finding was due to several things, with one of them being poor performance status. Based on ATA recommendations, ATC patients who have undergone R0 and R1 surgery, with good performance status and no evidence of metastasis, can be advised of an aggressive approach with intensity-modulated radiotherapy (IMRT) and systemic therapy which showed better survival [3]. However, 64.3% of patients in this study had poor performance status and 40.5% had distant metastasis which causes aggressive therapeutic options to be limited. Furthermore, the application of multimodal therapy to ATC patients in this research center is not always possible due to limited resources and low levels of health awareness among patients, so they often come at an advanced stage.
However, several previous studies have shown that an aggressive approach with multimodal therapy has shown increased survival in ATC patients. Nachalon et al found that patients who received curative RT (dose 70 Gy) showed a longer survival time (11 months), compared to patients with an aggressive palliative RT approach (dose 50 Gy) (6 months), palliative RT (dose ≤ 30 Gy) (3 months), and no therapy (1 month). The same study also showed that patients who received chemotherapy had a longer survival than patients who did not receive chemotherapy (11 vs. 4 months). This suggests that an aggressive approach with RT can prolong patient survival even in patients with metastases (stage IVc), without causing significant side effects [17].
In ATC patients, the goal of management can be therapeutic and/or palliative depending on the stage and prognosis of the patient. One of the currently recommended therapeutic approaches is multimodal therapy which combines surgery, RT, chemotherapy, and/or targeted therapy [11]. This study found that only five patients received multimodal therapy consisting of surgery and chemotherapy or RT. A total of 11 patients in this study have died before receiving surgery or chemotherapy/RT. The 2021 ATA consensus recommends complete tumor resection (R0/R1 surgery) for patients with stage IVa/IVb disease followed by IMRT and systemic therapy if the performance status is good and there is no evidence of metastasis. Meanwhile, patients who have undergone debulking resection (R2 surgery) or unresectable disease and have a good performance status can be offered IMRT and systemic therapy or a combination with BRAF/MEK inhibitors if they have positive BRAFV600E mutations. In patients with unresectable disease at diagnosis and who have the potential to become resectable with RT and/or systemic therapy, surgery should be reconsidered [3]. This was in line with this study’s findings which showed that patients who received combination therapy such as surgery + chemotherapy/RT had longer survival time, compared to the surgery or chemotherapy/RT only and un-therapied patients, even though it was not statistically significant.
The recommended surgery for patients with resectable tumors is total thyroidectomy. In this study, only 19.2% of patients could undergo total thyroidectomy, while the rest underwent partial resection. This caused most of the patients in this study to come with a terminal state condition which made the definitive radical surgery like total thyroidectomy not always available. The most common surgical modality being taken was the isthmectomy or isthmolobectomy as palliative surgery to remove thyroid mass, reduce pain, and prevent compression to the trachea or esophagus [18]. Another surgical approach found in this study was tracheostomy (19.2%) or a combination of isthmectomy + tracheostomy (26.9%) or total thyroidectomy + tracheostomy (7.8%). This condition is caused by airway disorders which are one of the common complaints found in ATC patients. Tashima et al found that at least 40% of ATC patients require tracheostomy [19]. Although intended as a life-saving procedure in patients with airway obstruction, tracheostomy is associated with decreased survival due to more aggressive tumor development or delayed onset of RT [3].
Apart from surgery, chemotherapy and RT are the main treatment options for ATC patients [3, 20]. This study found that 11.9% of patients underwent a combination of chemotherapy and/or RT, having a better median survival compared to patients who underwent surgery only. A study by Park et al found that IMRT provided better progression-free survival (PFS) and OS compared to three-dimensional conformal radiotherapy (3D-CRT) [21]. Another study by Jacob et al found that RT with a dose of 50 Gy or more provided a longer OS (13 months) compared to surgery only (9.8 months) (P < 0.05) [22]. In the postoperative setting, Kwon et al found that RT reduced the risk of death in postoperative ATC patients, compared to patients who underwent surgery alone (hazard ratio = 0.556; 95% confidence interval (CI): 0.419 - 0.737) [23]. Furthermore, the main purpose of chemotherapy combined with RT is to increase the possibility of local tumor control and the effect of tumor cytoreduction which aims to control the presence of systemic micrometastasis [3]. A study by Wang et al found that the combination of chemotherapy with RT showed a median OS of 6 months and a median PFS of 3.2 months. The study also found that the objective response rate (ORR) and disease control rate (DCR) of patients who received the combination reached 21% and 64% [24].
One of the current approaches in the management of ATC is by administering targeted therapy in the form of BRAF/MEK inhibitors. This is because BRAF mutations can be found in 40-70% of ATC cases. Immunohistochemistry (IHC) examination of BRAFV600E mutations can help establish the diagnosis of ATC and determine the choice of therapy [25, 26]. Phase 2 clinical trials showed that the administration of BRAF inhibitors (dabrafenib) and MEK inhibitors (trametinib) provided significant response rate results in ATC patients and have been approved by the United States Food and Drug Administration (FDA) [27]. Another study by Keam et al also found that the combination of dabrafenib + trametinib in BRAFV600E mutation-positive ATC patients showed an ORR of 67%, with a median PFS of 1.2 years, while the median OS was 1.7 years [28].
However, this study also has several limitations. Even though this study included patients for 27 years, it still lacks data to gather, due to the low prevalence of ATC in the community. This study also did not evaluate the disease-free survival due to the short duration of observation on each patient. This may be caused by lack of facility which made a long wait for the patients to get the treatment. Nevertheless, this study still has important value on how aggressive this type of thyroid cancer is and provides data regarding the effect of different therapeutic modalities on its prognosis, especially in LMIC settings. Our center also will continue to observe and record ATC cases in the future.
Conclusion
Survival rates of ATC have remained low and aggressive strategies are still needed to improve the prognosis of ATC. Further research is needed to find new therapeutic modalities for ATC.
Acknowledgments
The authors would like to thank all who contributed in helping this manuscript.
Financial Disclosure
There is nothing to declare.
Conflict of Interest
There is nothing to declare.
Informed Consent
Not applicable.
Author Contributions
PATA: project development, data collection, data analysis, manuscript writing and editing. GBS and IWS: data collection, manuscript writing and editing. IPGSS: data collection, data analysis, manuscript writing and editing.
Data Availability
The data supporting the findings of this study are available from the corresponding author upon reasonable request.
Abbreviations
AJCC: American Joint Committee on Cancer; ATA: American Thyroid Association; ATC: anaplastic thyroid carcinoma; IMRT: intensity-modulated radiotherapy; RT: radiotherapy
| References | ▴Top |
- Molinaro E, Romei C, Biagini A, Sabini E, Agate L, Mazzeo S, Materazzi G, et al. Anaplastic thyroid carcinoma: from clinicopathology to genetics and advanced therapies. Nat Rev Endocrinol. 2017;13(11):644-660.
doi pubmed - Ito K, Hanamura T, Murayama K, Okada T, Watanabe T, Harada M, Ito T, et al. Multimodality therapeutic outcomes in anaplastic thyroid carcinoma: improved survival in subgroups of patients with localized primary tumors. Head Neck. 2012;34(2):230-237.
doi pubmed - Bible KC, Kebebew E, Brierley J, Brito JP, Cabanillas ME, Clark TJ, Jr., Di Cristofano A, et al. 2021 American Thyroid Association Guidelines for management of patients with anaplastic thyroid cancer. Thyroid. 2021;31(3):337-386.
doi pubmed - Jimenez-Fonseca P, Gomez Saez JM, Santamaria Sandi J, Capdevila J, Navarro Gonzalez E, Zafon Llopis C, Ramon YCAT, et al. Spanish consensus for the management of patients with anaplastic cell thyroid carcinoma. Clin Transl Oncol. 2017;19(1):12-20.
doi pubmed - Fan D, Ma J, Bell AC, Groen AH, Olsen KS, Lok BH, Leeman JE, et al. Outcomes of multimodal therapy in a large series of patients with anaplastic thyroid cancer. Cancer. 2020;126(2):444-452.
doi pubmed - Niu Y, Ding Z, Deng X, Guo B, Kang J, Wu B, Fan Y. A novel multimodal therapy for anaplastic thyroid carcinoma: (125) I seed implantation plus Apatinib after surgery. Front Endocrinol (Lausanne). 2020;11:207.
doi pubmed - Guo H, Lin H. The value of multimodal treatment in anaplastic thyroid cancer patients with distant metastasis. BMC Surg. 2024;24(1):79.
doi pubmed - Pavlidis ET, Galanis IN, Pavlidis TE. Update on current diagnosis and management of anaplastic thyroid carcinoma. World J Clin Oncol. 2023;14(12):570-583.
doi pubmed - Alhejaily AG, Alhuzim O, Alwelaie Y. Anaplastic thyroid cancer: pathogenesis, prognostic factors and genetic landscape (Review). Mol Clin Oncol. 2023;19(6):99.
doi pubmed - Janz TA, Neskey DM, Nguyen SA, Lentsch EJ. Is the incidence of anaplastic thyroid cancer increasing: A population based epidemiology study. World J Otorhinolaryngol Head Neck Surg. 2019;5(1):34-40.
doi pubmed - Jannin A, Escande A, Al Ghuzlan A, Blanchard P, Hartl D, Chevalier B, Deschamps F, et al. Anaplastic thyroid carcinoma: an update. Cancers (Basel). 2022;14(4):1061.
doi pubmed - Kong N, Xu Q, Zhang Z, Cui A, Tan S, Bai N. Age influences the prognosis of anaplastic thyroid cancer patients. Front Endocrinol (Lausanne). 2021;12:704596.
doi pubmed - Zivaljevic V, Tausanovic K, Paunovic I, Diklic A, Kalezic N, Zoric G, Sabljak V, et al. Age as a prognostic factor in anaplastic thyroid cancer. Int J Endocrinol. 2014;2014:240513.
doi pubmed - Rao SN, Smallridge RC. Anaplastic thyroid cancer: An update. Vol. 37. Best practice and research: clinical endocrinology and metabolism. Bailliere Tindall Ltd; 2023.
- Zarg El Ayoun R, Chtourou MF, Beji H, Kchaou M, Belfekih H, Chelbi E, Mighri MM, et al. A pancreatic metastasis of anaplastic thyroid carcinoma: a rare case report. Ann Med Surg (Lond). 2023;85(2):228-230.
doi pubmed - Smallridge RC, Ain KB, Asa SL, Bible KC, Brierley JD, Burman KD, Kebebew E, et al. American Thyroid Association guidelines for management of patients with anaplastic thyroid cancer. Thyroid. 2012;22(11):1104-1139.
doi pubmed - Nachalon Y, Stern-Shavit S, Bachar G, Shvero J, Limon D, Popovtzer A. Aggressive palliation and survival in anaplastic thyroid carcinoma. JAMA Otolaryngol Head Neck Surg. 2015;141(12):1128-1132.
doi pubmed - Patel S, Goldenberg D, Bann DV. The role of surgery in the management of anaplastic thyroid carcinoma. Vol. 32, Operative Techniques in Otolaryngology - Head and Neck Surgery. W.B. Saunders; 2021. p. e27-e31.
- Tashima L, Mitzner R, Durvesh S, Goldenberg D. Dyspnea as a prognostic factor in anaplastic thyroid carcinoma. Eur Arch Otorhinolaryngol. 2012;269(4):1251-1255.
doi pubmed - Sekihara K, Himuro H, Toda S, Saito N, Hirayama R, Suganuma N, Sasada T, et al. Recent trends and potential of radiotherapy in the treatment of anaplastic thyroid cancer. Biomedicines. 2024;12(6):1286.
doi pubmed - Park JW, Choi SH, Yoon HI, Lee J, Kim TH, Kim JW, Lee IJ. Treatment outcomes of radiotherapy for anaplastic thyroid cancer. Radiat Oncol J. 2018;36(2):103-113.
doi pubmed - Jacob J, Vordermark D, Lorenz K, Medenwald D. Prognostic factors in radiotherapy of anaplastic thyroid carcinoma: a single center study over 31 years. Radiat Oncol. 2023;18(1):71.
doi pubmed - Kwon J, Kim BH, Jung HW, Besic N, Sugitani I, Wu HG. The prognostic impacts of postoperative radiotherapy in the patients with resected anaplastic thyroid carcinoma: A systematic review and meta-analysis. Eur J Cancer. 2016;59:34-45.
doi pubmed - Wang BC, Lin GH, Kuang BH, Cao RB. Emerging chemotherapy-based treatments in anaplastic thyroid cancer: an updated analysis of prospective studies. Front Endocrinol (Lausanne). 2024;15:1385747.
doi pubmed - Landa I, Ibrahimpasic T, Boucai L, Sinha R, Knauf JA, Shah RH, Dogan S, et al. Genomic and transcriptomic hallmarks of poorly differentiated and anaplastic thyroid cancers. J Clin Invest. 2016;126(3):1052-1066.
doi pubmed - Smith AL, Williams MD, Stewart J, Wang WL, Krishnamurthy S, Cabanillas ME, Roy-Chowdhuri S. Utility of the BRAF p.V600E immunoperoxidase stain in FNA direct smears and cell block preparations from patients with thyroid carcinoma. Cancer Cytopathol. 2018;126(6):406-413.
doi pubmed - Subbiah V, Kreitman RJ, Wainberg ZA, Gazzah A, Lassen U, Stein A, Wen PY, et al. Dabrafenib plus trametinib in BRAFV600E-mutated rare cancers: the phase 2 ROAR trial. Nat Med. 2023;29(5):1103-1112.
doi pubmed - Keam B, Kreitman RJ, Wainberg ZA, Cabanillas ME, Cho DC, Italiano A, et al. Updated efficacy and safety data of dabrafenib (D) and trametinib (T) in patients (pts) with BRAF V600E-mutated anaplastic thyroid cancer (ATC). In: Annals of Oncology. Elsevier BV; 2018. p. viii645-vii646.
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
World Journal of Oncology is published by Elmer Press Inc.