| World Journal of Oncology, ISSN 1920-4531 print, 1920-454X online, Open Access |
| Article copyright, the authors; Journal compilation copyright, World J Oncol and Elmer Press Inc |
| Journal website https://www.wjon.org |
Original Article
Volume 15, Number 6, December 2024, pages 942-949
Clinicopathological Factors and Interleukin-6 Levels Associated With Low Relative Dose Intensity in Women With Breast Cancer Receiving First-Line Chemotherapy
Susanna Hilda Hutajulua, h, Yufi Kartika Astarib, Meita Ucchec, Dewi Kartikawati Paramitad, Riani Witaningrume, Rizka Humardewayanti Asdief, Raden Bowo Pramonog, Mardiah Suci Hardiantia, Kartika Widayati Taroeno-Hariadia, Ibnu Purwantoa, Johan Kurniandaa
aDivision of Hematology and Medical Oncology, Department of Internal Medicine, Faculty of Medicine, Public Health and Nursing, Universitas Gadjah Mada/Dr. Sardjito General Hospital, Yogyakarta, Indonesia
bDivision of Hematology and Medical Oncology, Department of Internal Medicine, Dr. Sardjito General Hospital, Yogyakarta, Indonesia
cStudy Program of Specialty in Internal Medicine, Department of Internal Medicine, Faculty of Medicine, Public Health and Nursing, Universitas Gadjah Mada/Dr. Sardjito General Hospital, Yogyakarta, Indonesia
dDepartment of Histology and Cell Biology, Faculty of Medicine, Public Health and Nursing, Universitas Gadjah Mada, Yogyakarta, Indonesia
eDepartment of Nutrition and Health, Faculty of Medicine, Public Health and Nursing, Universitas Gadjah Mada, Yogyakarta, Indonesia
fDivision of Tropical Medicine and Infectious Disease, Department of Internal Medicine, Faculty of Medicine, Public Health and Nursing, Universitas Gadjah Mada/Dr. Sardjito General Hospital, Yogyakarta, Indonesia
gDivision of Endocrinology, Department of Internal Medicine, Faculty of Medicine, Public Health and Nursing, Universitas Gadjah Mada/Dr. Sardjito General Hospital, Yogyakarta, Indonesia
hCorresponding Author: Susanna Hilda Hutajulu, Division of Hematology and Medical Oncology, Department of Internal Medicine, Faculty of Medicine, Public Health and Nursing, Universitas Gadjah Mada/Dr. Sardjito General Hospital, Yogyakarta 55284, Indonesia
Manuscript submitted September 2, 2024, accepted October 22, 2024, published online October 30, 2024
Short title: Low RDI in BC Chemotherapy
doi: https://doi.org/10.14740/wjon1954
| Abstract | ▴Top |
Background: Chemotherapy has a substantial role in decreasing the risk of recurrence and mortality in breast cancer (BC) in a dose-dependent manner where a low relative dose intensity (RDI) is associated with unfavorable outcomes. Several baseline clinicopathological factors, including pro-inflammatory biomarkers, were found to be significant determinants of low RDI. This study aimed to explore the occurrence of low RDI and its influencing factors in women with BC.
Methods: This cross-sectional study recruited 172 women with stage I-IV BC who received first-line chemotherapy. We collected patients’ clinical, pathological, and treatment data and analyzed the pre-chemotherapy C-reactive protein (CRP) and interleukin (IL)-6 levels using a quantitative enzyme-linked immunosorbent assay (ELISA). We calculated the RDI based on the actual and planned delivered chemotherapy dose (mg/m2) and duration (weeks). RDI less than 85% was defined as “low”. Multivariate analysis with logistic regression was conducted to determine the association between pre-chemotherapy parameters and RDI < 85%.
Results: The mean CRP level was 10.82 ± 19.17 mg/L (0.00 - 151.73 mg/L) and the mean IL-6 level was 1.12 ± 3.41 pg/mL (0.00 - 27.67 pg/mL). The average RDI for all patients was 93±8.19%. An RDI < 85% occurred in 23 patients (13.4%). The presence of diabetes mellitus (odds ratio (OR): 4.78, 95% confidence interval (CI): 1.03 - 22.27, P = 0.046), triple-negative tumors (OR: 6.45, 95% CI: 1.39 - 29.83, P = 0.017), and IL-6 levels > 0.5 pg/mL (OR: 3.45, 95% CI: 1.01 - 11.79, P = 0.049) was associated with an increased low RDI risk.
Conclusion: The proportion of BC patients receiving a low chemotherapy RDI in our study was comparable to published literature and drove close monitoring of patients at risk to provide adequate management.
Keywords: Breast neoplasms; Chemotherapy; Inflammation; Interleukin-6
| Introduction | ▴Top |
Chemotherapy has a substantial role in decreasing the risk of recurrence and mortality in breast cancer (BC) [1]. The greatest benefits are obtained from chemotherapy regimens with higher cumulative dose intensity or in a dose-dependent manner [1, 2]. However, in addition to damaging cancer cells, chemotherapy comes with the risk of hematological and non-hematological toxicities, experienced by a large number of patients [3, 4]. The occurrence of severe toxicities such as febrile neutropenia, severe neutropenia, anemia, and thrombocytopenia can lead to reduced relative dose intensity (RDI) in particular patients [2].
A low RDI or RDI < 85% is associated with unfavorable overall survival (OS) in cases with colorectal, pancreatic, ovarian, lung, and breast cancer (hazard ratio (HR): 1.17 - 1.39) [2]. Particularly in BC, RDI < 85% significantly correlated with worse disease-free survival (DFS) in non-metastatic patients (HR: 1.45 - 1.97) [5, 6], and shorter OS in metastatic cases (HR: 1.32) [7]. A study focusing on BC cases with human epidermal growth factor receptor 2 (HER2)-negative tumors showed that 5-year OS was lower in patients who received RDI < 85% compared to RDI ≥ 85% (76.3% vs. 91.2%, P = 0.015) [8].
Apart from hematological and non-hematological toxicities that have been observed in relation to low RDI, several baseline clinicopathological and treatment factors were found to be significant determinants of low RDI in BC, including age [9-12], body mass index (BMI) [13, 14], body surface area (BSA) [11, 12], comorbidity presence [11], tumor stage [15], molecular subtype [15], and anthracycline-based regimen [11]. There is also growing evidence demonstrating that pro-inflammatory biomarkers, including C-reactive protein (CRP), interleukin (IL)-6, IL-8, and tumor necrosis factor-alpha (TNF-α), had an association with reduced RDI [9, 16].
Since maintaining RDI is essential to achieve better outcomes, it is important to identify BC patients who are at risk of receiving a reduced RDI. The inconsistent observations among studies investigating the association between pro-inflammatory biomarkers and RDI also need to be addressed. The objective of this study was to determine whether baseline clinicopathological, treatment, and pro-inflammatory parameters are associated with a reduced RDI in women with BC.
| Materials and Methods | ▴Top |
Study participants and design
This cross-sectional study recruited women with BC who received first-line chemotherapy and were enrolled in a prospective cohort study investigating BC chemotoxicity. Participants were BC patients visiting the Hematology and Medical Oncology Division, “Tulip”/Integrated Cancer Clinic, Dr. Sardjito General Hospital, Yogyakarta, Indonesia, between July 2018 and March 2022. Women with histopathologically confirmed BC, aged 18 years or older, with an Eastern Cooperative Oncology Group (ECOG) performance status of ≤ 2, no history of previous chemotherapy, and without a fatal illness or severe congestive heart failure were enrolled in the main study. Patients were excluded from the present study if: 1) they had not received at least three cycles of chemotherapy; 2) they received a non-3-weekly chemotherapy regimen; or 3) they did not have stored pre-chemotherapy blood samples. A total of 172 patients were eventually included in the present study. The study was authorized by the Medical and Health Research and Ethics Committee, Faculty of Medicine, Public Health and Nursing, Universitas Gadjah Mada (reference number: KE/FK/0417/EC/2018), and was conducted in compliance with the ethical standards of the responsible institution on human subjects as well as with the Helsinki Declarations. All participants provided written consent prior to study enrolment.
Clinical, pathological, and treatment characteristics
Patients’ clinical, pathological, and treatment data were retrieved from the main study database from August to December 2023. The baseline clinical data consisted of age (< 60 years vs. ≥ 60 years), BMI (< 23 kg/m2 vs. ≥ 23 kg/m2 based on WHO BMI cut-off for Asians), comorbidity presence (yes vs. no, including at least one of these following comorbidities: diabetes mellitus, hypertension, dyslipidemia, hyperuricemia, gastritis, asthma, or allergy), diabetes mellitus comorbidity (yes vs. no), hypertension comorbidity (yes vs. no), and pre-treatment laboratory parameters including glucose (mg/dL), albumin (g/dL), and vitamin D (ng/mL). Baseline tumor and pathological data included cancer stage (stage I-II vs. stage III-IV based on the eighth edition AJCC staging system), and estrogen receptors (ER), progesterone receptors (PR), and human epidermal growth factor receptor 2 (HER2) status (ER+ or PR+, HER2- vs. HER2+ vs. ER-, PR-, HER2-). Last, the treatment data consisted of chemotherapy setting (adjuvant and neoadjuvant vs. palliative) and chemotherapy regimen (anthracycline plus cyclophosphamide (AC), taxane (T), anthracycline plus cyclophosphamide followed by taxane (AC-T) and capecitabine).
Pro-inflammatory biomarkers
CRP and IL-6 levels were analyzed using a quantitative enzyme-linked immunosorbent assay (ELISA) on pre-chemotherapy blood samples stored in Biobank, Faculty of Medicine, Public Health, and Nursing, Universitas Gadjah Mada. Prior to the initiation of chemotherapy, peripheral blood (21 mL) was collected. After centrifugation, plasma samples were aliquoted and stored at -80 °C until analysis. Quantitative pro-inflammatory biomarker measurements included high-sensitivity CRP (Calbiotech, El Cajon, California, Catalog No. CR120C) and human IL-6 (Elabscience, Houston, TX, Catalog No. E-EL-H6156). Analysis was done at the Integrated Research Laboratory, Faculty of Medicine, Public Health, and Nursing, Universitas Gadjah Mada by trained laboratory staff blinded to patients’ characteristics.
RDI
RDI is the ratio of the total delivered dose (mg/m2) divided by actual time to complete delivered chemotherapy (weeks) to the total intended dose (mg/m2) divided by standard time to complete intended chemotherapy regimen (weeks), ranging from 0 to 100%. A dose delay or dose reduction can cause decreases in RDI [17, 18]. For chemotherapy regimen containing multiple agents, RDI was the mean value of the individual RDIs from each agent in the chemotherapy regimen. RDI less than 85% was defined as “low” [19].
Statistical analysis
Patients’ clinical, pathological, and treatment characteristics were described as mean and standard deviation (SD) or frequency and percentage. Pro-inflammatory biomarkers were presented as mean, SD, minimum and maximum value, clinical cut-off and the area under the receiving operating characteristics (ROC) curve (AUC).
Pre-treatment laboratory parameters and pro-inflammatory biomarkers were grouped based on cut-off value using the Liu Index method to maximize the AUC. Considering optimal clinical practice application, rounded cut-off values were chosen. Univariate and multivariate analysis with logistic regression was conducted to determine the association between pre-chemotherapy parameters and RDI < 85%. All parameters with a P value under 0.250 were included in the multivariate analysis. A P value under 0.05 was considered significant. The statistical analyses were performed with Stata version 17 (Stata Corp., College Station, TX).
| Results | ▴Top |
Baseline characteristics
From 245 patients in the main study, 73 patients were excluded due to not receiving chemotherapy (n = 36), receiving less than three chemotherapy cycles (n = 15), not having a 3-weekly chemotherapy regimen (n = 1), incomplete clinical data (n = 2), and not having blood sample stored (n = 19). A total of 172 patients with stage I-IV BC were included in this study (Fig. 1). The mean age of patients was 52 years (range 32 - 78 years). Among them, 82.0% were equal to or under 60 years old, 55.8% had normal to underweight BMI, and 57.6% had at least one comorbidity. Most patients were diagnosed with stage III-IV BC (69.8%), were ER+ or PR+ and HER2- (49.4%), and received AC-T regimen (71.5%) (Table 1).
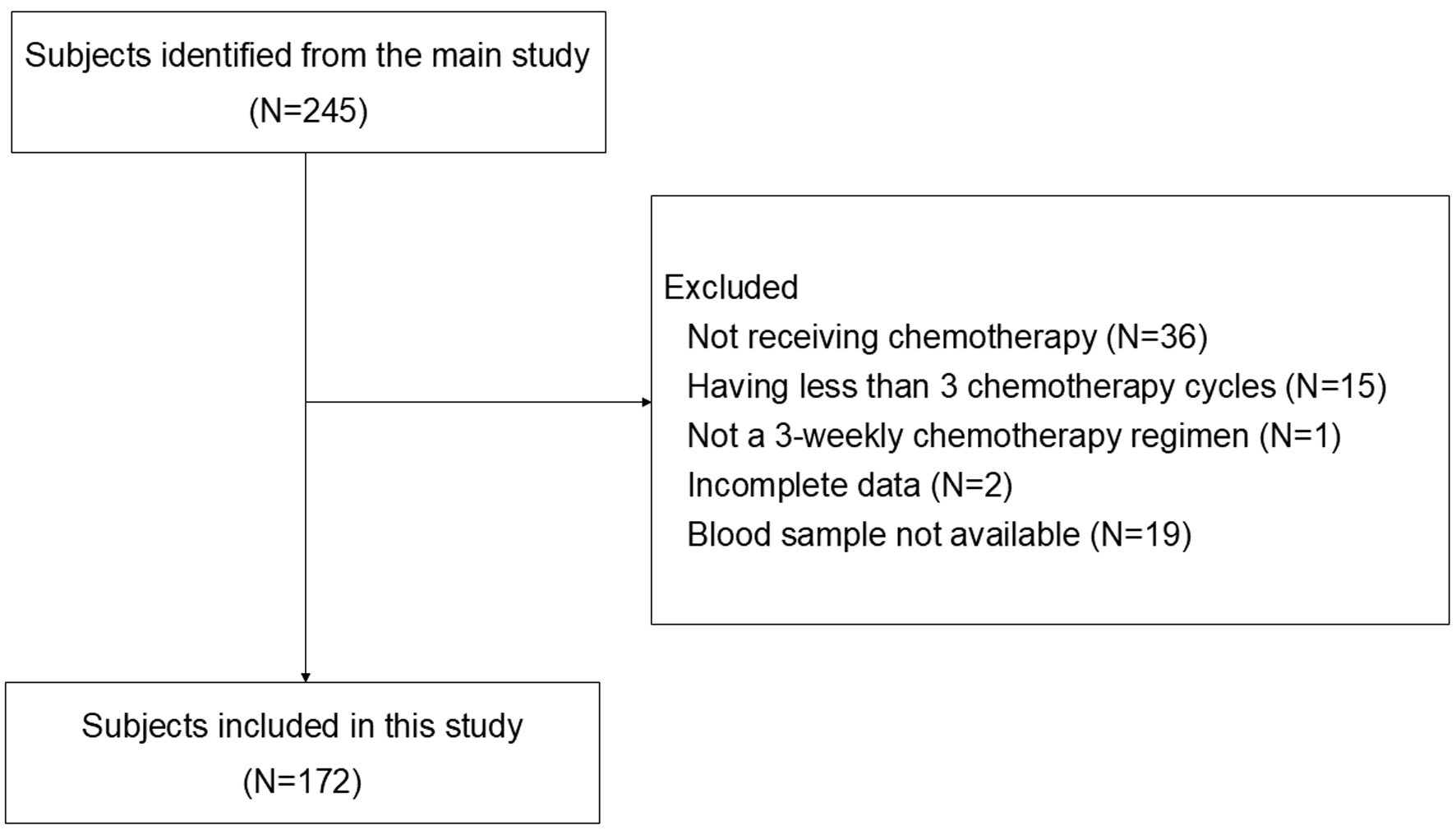 Click for large image | Figure 1. Flowchart of subjects’ inclusion. From 245 patients in the main study, 73 patients were excluded due to not receiving chemotherapy, receiving less than 3 chemotherapy cycles, not having 3-weekly chemotherapy regimen, incomplete clinical data, and unavailability of stored blood sample. A total of 172 patients with stage I-IV BC were included for analysis. |
 Click to view | Table 1. Baseline Characteristics (N = 172) |
Pro-inflammatory biomarkers
The mean CRP level was 10.82 ± 19.17 mg/L, with a median value of 5.02 mg/L (range 0.00 - 151.73 mg/L). The mean IL-6 level was 1.12 ± 3.41 pg/mL (range 0.00 - 27.67 pg/mL). Based on Liu Index methods, this study used 5 mg/L (AUC: 0.53) and 0.5 pg/mL (AUC: 0.66) as the clinical cut-off for CRP and IL-6.
Factors associated with a low RDI
The average RDI for all patients was 93±8.19%, and an RDI < 85% occurred in 23 patients (13.4%). The average RDI was 92±10.37% for patients receiving AC regimen, 91±9.95% for patients receiving taxane regimen, 93±7.26% for patients receiving AC-T regimen, and 93±11.4% for patients receiving capecitabine regimen.
In the univariate analysis, diabetes mellitus comorbidity (P = 0.005), palliative chemotherapy setting (P = 0.003), and IL-6 levels > 0.5 pg/mL (P = 0.001) were significantly associated with RDI < 85% (Table 2). With a P value less than 0.250, BMI, comorbidity presence, cancer stage, ER, PR, HER2 status, chemotherapy regimen, glucose, and albumin levels were also included in the multivariable analysis. In the multivariable analysis, factors associated with a low RDI risk were the presence of diabetes mellitus comorbidity (odds ratio (OR): 4.78, 95% confidence interval (CI): 1.03 - 22.27, P = 0.046), ER-, PR-, HER2- or triple-negative tumors (OR: 6.45, 95% CI: 1.39 - 29.83, P = 0.017), and IL-6 levels > 0.5 pg/mL (OR: 3.45, 95% CI: 1.01 - 11.79, P = 0.049).
 Click to view | Table 2. Clinicopathological and Pro-Inflammatory Factors Associated With RDI < 85% |
| Discussion | ▴Top |
This study was one of the few investigating pro-inflammatory biomarkers and other determinant factors of low RDI in BC chemotherapy. In the present study, the average RDI of chemotherapy in (neo)adjuvant and palliative settings was 93%. As much as 13.4% of patients received RDI less than 85%. Patients with diabetes mellitus, triple-negative tumors, and pre-treatment IL-6 level > 0.5 pg/mL faced a higher risk of low RDI of BC chemotherapy when compared with their counterparts.
Our study observed a comparable low RDI occurrence with previous studies on BC chemotherapy dose intensity from Thailand, Sweden, Australia, and the UK (11.6-17%) [13, 16]. The last two studies also reported a similar RDI average of 92% and 95% [10, 14]. A study from the Netherlands that enrolled stage I-III BC patients found fewer patients experiencing a low RDI (9.6%) given that the average RDI administered was higher than ours (99% vs. 93%) [20]. Meanwhile, with a lower RDI average (79.4-88%) than ours, previous studies from the USA reported a higher low RDI occurrence (30-55.5%) [11, 12, 21, 22]. The proportion of patients receiving substandard chemotherapy dose intensity in our study drove the provision of more adequate management, especially for patients at risk.
We found that diabetes mellitus was significantly associated with a higher risk of low RDI in contrast to a previous study in colorectal cancer patients that showed no significant correlation between them [23]. We proposed that hyperglycemia, as a classic feature of diabetes mellitus, was associated with chemotherapy dose modification and RDI reduction [17, 18]. During chemotherapy, steroids are often administered as pre-medication to prevent allergic reactions caused by chemotherapy agents. Through several mechanisms including downregulation of glucose transporter 4 (GLUT4) in muscle, increased glucose production in the liver, insulin receptor binding inhibition, and decreased insulin secretion, steroids affect glucose metabolism and insulin resistance leading to hyperglycemia [24]. Hyperglycemia is frequently observed during chemotherapy [25], leading to a dose delay. Dose delay was defined as a delay of 7 or more days in administering at least one chemotherapy agent relative to the standard [12], as we also commonly see in our previous report [26]. In our study population, dose delay was found in 77 (44.8%) patients. Among patients with diabetes mellitus, 13 (65%) patients experienced dose delay. We found that patients with diabetes mellitus tend to have a higher risk of experiencing dose delay throughout chemotherapy cycles compared to patients without diabetes mellitus (65% vs. 42.1%, P = 0.053) (Supplementary Material 1, wjon.elmerpub.com) which is responsible for a low RDI occurrence.
Another study observed that BC patients with diabetes mellitus had an increased risk of chemotherapy toxicities, including neutropenia, anemia, thrombocytopenia, and infection or fever, through several mechanisms [27]. Diabetes mellitus has impacts on nerves and vascular structures, insulin-like growth factor 1 (IGF-1) activation, drug pharmacokinetics, including anthracycline and taxane, and expression levels of hepatic CYP450 and Mdr1b that induce drug toxicity [28]. The odds of experiencing neutropenia were 32% higher in patients with diabetes mellitus due to impaired neutrophil function, defects in chemotaxis and hematopoietic progenitor that increased bone marrow suppression [28, 29]. Even though diabetes mellitus was well-controlled and asymptomatic, there was a microvascular disorder associated with platelet dysfunction. Platelets adhered to vascular endothelium and aggregated more than in non-diabetic patients causing thrombocytopenia [30]. Increased toxicity occurrence during chemotherapy leads to a lower dose, a less aggressive, or early discontinuation of chemotherapy, which contributes to a low RDI [27]. Previous study also demonstrated that grade 3-4 neutropenia significantly increased the probability of having RDI < 85% by 74% [3].
Our observation of a higher risk of low RDI in triple-negative BC cases is in line with a previous study reporting a lower RDI < 85% occurrence in hormone receptor-positive BC [15], although others did not find such differences [9, 16]. The triple-negative tumor has been reported to have a better response rate to chemotherapy than hormone receptor-positive BC due to its higher proliferation rate. A study indicated that hormone receptor-positive BC patients should avoid reducing RDI lower than 85% to maintain survival benefits, while the cut-off is lower than 75% in triple-negative BC patients [18]. Thus, it is expected that the chance of having a low RDI is higher in triple-negative BC.
Notably, we found that IL-6, as a marker of inflammation, was linked to a higher low RDI risk. The association of inflammation and RDI in BC patients has been addressed in two previous studies. Yuan et al [9] showed an association between low RDI and pre-treatment IL-6, while Schauer et al [16] found a significant association between low RDI and pre-treatment IL-8 and TNF-α, but not with IL-6. Given that IL-6 levels increase with age or act as ageing biomarkers, the latter hypothesized that the absence of correlation between RDI and IL-6 was because their participants were younger [9, 16]. The role of IL-6 as an ageing biomarker was also seen in this study, as we found that patients with IL-6 levels > 0.5 pg/mL were older (56 vs. 51 years, P = 0.003) (Supplementary Material 2, wjon.elmerpub.com). However, despite having younger participants (52 vs. 59 years old) and lower IL-6 levels (mean 1.12 vs. 3.4 pg/mL) compared to Yuan et al [9], we were still able to observe that IL-6 > 0.5 pg/mL was significantly associated with a low RDI risk.
Elevated pre-treatment IL-6 levels have been observed to correlate with advanced cancer stage and poorer response to chemotherapy [9]. In addition to objectives of the present study, we observed that pre-treatment IL-6 > 0.5 pg/mL was associated with stage 4 disease (OR: 5.85, 95% CI: 2.60 - 13.14, P < 0.001) and unfavorable post-chemotherapy response (OR: 3.58, 95% CI: 1.65 - 7.76, P = 0.001) (Supplementary Material 3 and 4, wjon.elmerpub.com). Furthermore, along with other biomarkers such as CRP and albumin, IL-6 levels were also found to correlate with an increased risk of chemotoxicity [16], particularly cancer-related fatigue [31]. A high IL-6 level stimulates the increase of hepcidin, which affects the efficiency of oxygenation and leads to fatigue in BC patients [32]. Among 23 patients who received low RDI in our cohort, 39.1% of patients experienced severe fatigue at any chemotherapy cycle. Other non-hematological and hematological chemotherapy toxicities were also observed, including severe nausea-vomiting (17.4%), severe neutropenia (65.2%), severe anemia (56.5%), and severe thrombocytopenia (13.1%). Further analysis did not show any significant association between chemotherapy toxicities and a reduced RDI (Supplementary Material 5, wjon.elmerpub.com).
Our present study observed potential utilization of IL-6 measurement before chemotherapy to provide additional information for oncologists to identify patients who are at risk of receiving a low RDI. Despite of its availability, inflammatory biomarker measurement, including IL-6, has not been integrated in routine clinical practice for the local patients with BC. To actually incorporate routine IL-6 measurement into the national healthcare insurance setting, further advocation is warranted.
The strength of this study was the inclusion of various determinant factors in addition to classic risk factors. These included baseline inflammation biomarkers, albumin as a nutritional biomarker, and a relatively novel parameter in cancer, vitamin D. Nevertheless, albumin and vitamin D impacts on RDI were not observed. We also presented all laboratory variables as a rounded cut-off with a sensitive Liu method to optimize their applicability in daily clinical practices.
Limitations of this study include a single-center setting where careful consideration is needed to interpret the results. A low RDI was caused by dose reduction or dose delay during chemotherapy administration. While dose reduction is often caused by chemotherapy toxicity, a dose delay can happen due to hematological and non-hematological toxicities, or other socioeconomic factors including public holidays or patient preference.
Conclusions
This study observed that 13.4% of BC patients received an RDI less than 85%. Patients with diabetes mellitus, triple-negative tumors, and IL-6 serum levels > 0.5 pg/mL at baseline are susceptible to receiving a reduced RDI. This group of patients needs to be closely monitored to prevent suboptimal RDI administration.
| Supplementary Material | ▴Top |
Suppl 1. Association of diabetes mellitus comorbidity and dose delay.
Suppl 2. Association of baseline IL-6 level with patient’s age.
Suppl 3. Association of baseline IL-6 level with cancer stage.
Suppl 4. Association of baseline IL-6 level with treatment response after the first-line chemotherapy (complete response vs. non-complete response).
Suppl 5. Association of baseline hematological and non-hematological chemotoxicities and low RDI occurrence.
Acknowledgments
The authors thank Benedreky Leo, Irfan Haris, Norma Dewi Suryani, Betrix Rifana Kusuma, Refdiana Dewi, and Sumartiningsih for technical assistance.
Financial Disclosure
This work was supported by The Indonesian Ministry of Research, Technology, and Higher Education (2018, grant number: 1820/UN1/DITLIT/DIT-LIT/LT-2018 and 2020, grant number: 2258/UN1/DITLIT/DIT-LIT/PT/2020).
Conflict of Interest
The authors declare no conflict of interest.
Informed Consent
Written informed consent was obtained from the subject of the study for participation in the research.
Author Contributions
Conceptualization: SHH, RHA, RBP, MSH, KWT, IP, and JK. Data acquisition: SHH, YKA, MU, DKP, and RW. Formal analysis and interpretation: SHH, YKA, MU, and DKP. Writing original draft: SHH and YKA. Review and editing draft: MU, DKP, RW, RHA, RBP, MSH KWT, IP, and JK. All authors have read and agreed to the published version of the manuscript.
Data Availability
The data used in this study are available from the corresponding author upon reasonable request.
Abbreviations
AC: anthracycline/cyclophosphamide; AC-T: anthracycline/cyclophosphamide and taxane; AUC: area under the ROC curve; BC: breast cancer; BMI: body mass index; BSA: body surface area; CRP: C-reactive protein; DFS: disease-free survival; ECOG: Eastern Cooperative Oncology Group; ELISA: enzyme-linked immunosorbent assay; ER: estrogen receptor; GLUT4: glucose transporter 4; HER2: human epidermal growth factor receptor 2; IGF-1: insulin-like growth factor 1; IL-6: interleukin-6; PR: progesterone receptor; RDI: relative dose intensity; ROC: receiving operating characteristics; SD: standard deviation; T: taxane; TNF-α: tumor necrosis factor-alpha
| References | ▴Top |
- Early Breast Cancer Trialists' Collaborative Group . Electronic address bocoau, Early Breast Cancer Trialists' Collaborative G. Anthracycline-containing and taxane-containing chemotherapy for early-stage operable breast cancer: a patient-level meta-analysis of 100 000 women from 86 randomised trials. Lancet. 2023;401(10384):1277-1292.
doi pubmed - Nielson CM, Bylsma LC, Fryzek JP, Saad HA, Crawford J. Relative dose intensity of chemotherapy and survival in patients with advanced stage solid tumor cancer: a systematic review and meta-analysis. Oncologist. 2021;26(9):e1609-e1618.
doi pubmed - Gadisa DA, Assefa M, Tefera GM, Yimer G. Patterns of anthracycline-based chemotherapy-induced adverse drug reactions and their impact on relative dose intensity among women with breast cancer in Ethiopia: a prospective observational study. J Oncol. 2020;2020:2636514.
doi pubmed - Wiranata JA, Hutajulu SH, Astari YK, Leo B, Bintoro BS, Hardianti MS, Taroeno-Hariadi KW, et al. Patient-reported outcomes and symptom clusters pattern of chemotherapy-induced toxicity in patients with early breast cancer. PLoS One. 2024;19(2):e0298928.
doi pubmed - Veitch Z, Khan OF, Tilley D, Tang PA, Ribnikar D, Stewart DA, Kostaras X, et al. Impact of Cumulative Chemotherapy Dose on Survival With Adjuvant FEC-D Chemotherapy for Breast Cancer. J Natl Compr Canc Netw. 2019;17(8):957-967.
doi pubmed - Qi W, Wang X, Gan L, Li Y, Li H, Cheng Q. The effect of reduced RDI of chemotherapy on the outcome of breast cancer patients. Sci Rep. 2020;10(1):13241.
doi pubmed - Loibl S, Skacel T, Nekljudova V, Luck HJ, Schwenkglenks M, Brodowicz T, Zielinski C, et al. Evaluating the impact of Relative Total Dose Intensity (RTDI) on patients' short and long-term outcome in taxane- and anthracycline-based chemotherapy of metastatic breast cancer- a pooled analysis. BMC Cancer. 2011;11:131.
doi pubmed - Yamada A, Nakazawa K, Akazawa K, Narui K, Endo I, Hasegawa Y, Kohno N, et al. Impact of the relative dose intensity of neoadjuvant chemotherapy with anthracycline followed by Taxane on the survival of patients with human epidermal growth factor receptor 2-negative breast cancer: the JONIE1 study. Anticancer Res. 2021;41(2):1063-1068.
doi pubmed - Yuan Y, Vora N, Sun CL, Li D, Soto-Perez-de-Celis E, Mortimer J, Luu TH, et al. Association of pre-chemotherapy peripheral blood pro-inflammatory and coagulation factors with reduced relative dose intensity in women with breast cancer. Breast Cancer Res. 2017;19(1):101.
doi pubmed - Sandy J, Della-Fiorentina S. Relative dose intensity in early stage breast cancer chemotherapy: A retrospective analysis of incidence, risk factors and outcomes at a south-west Sydney cancer clinic. Asia Pac J Clin Oncol. 2013;9(4):365-372.
doi pubmed - Shayne M, Crawford J, Dale DC, Culakova E, Lyman GH, ANC Study Group. Predictors of reduced dose intensity in patients with early-stage breast cancer receiving adjuvant chemotherapy. Breast Cancer Res Treat. 2006;100(3):255-262.
doi pubmed - Lyman GH, Dale DC, Crawford J. Incidence and predictors of low dose-intensity in adjuvant breast cancer chemotherapy: a nationwide study of community practices. J Clin Oncol. 2003;21(24):4524-4531.
doi pubmed - Thanestada J, Srinonprasert V, Nimmannit A, Korphaisarn K, Pramyothin P, Akewanlop C. Low fat-free mass index measured by bioelectrical impedance analysis correlates with hematologic adverse events in early-stage breast cancer patients receiving chemotherapy: a prospective observational cohort study. Technol Cancer Res Treat. 2022;21:15330338221106529.
doi pubmed - Jenkins P, Elyan S, Freeman S. Obesity is not associated with increased myelosuppression in patients receiving chemotherapy for breast cancer. Eur J Cancer. 2007;43(3):544-548.
doi pubmed - Lyman GH, Dale DC, Tomita D, Whittaker S, Crawford J. A retrospective evaluation of chemotherapy dose intensity and supportive care for early-stage breast cancer in a curative setting. Breast Cancer Res Treat. 2013;139(3):863-872.
doi pubmed - Schauer T, Henriksson A, Strandberg E, Lindman H, Berntsen S, Demmelmaier I, Raastad T, et al. Pre-treatment levels of inflammatory markers and chemotherapy completion rates in patients with early-stage breast cancer. Int J Clin Oncol. 2023;28(1):89-98.
doi pubmed - Bretzel RL, Jr., Cameron R, Gustas M, Garcia MA, Hoffman HK, Malhotra R, Miller K, et al. Dose intensity in early-stage breast cancer: a community practice experience. J Oncol Pract. 2009;5(6):287-290.
doi pubmed - Zhang L, Yu Q, Wu XC, Hsieh MC, Loch M, Chen VW, Fontham E, et al. Impact of chemotherapy relative dose intensity on cause-specific and overall survival for stage I-III breast cancer: ER+/PR+, HER2- vs. triple-negative. Breast Cancer Res Treat. 2018;169(1):175-187.
doi pubmed - Weycker D, Barron R, Edelsberg J, Kartashov A, Lyman GH. Incidence of reduced chemotherapy relative dose intensity among women with early stage breast cancer in US clinical practice. Breast Cancer Res Treat. 2012;133(1):301-310.
doi pubmed - Schraa SJ, Frerichs KA, Agterof MJ, Hunting JCB, Los M, de Jong PC. Relative dose intensity as a proxy measure of quality and prognosis in adjuvant chemotherapy for breast cancer in daily clinical practice. Eur J Cancer. 2017;79:152-157.
doi pubmed - Griffin DA, Penprase B, Klamerus JF. Relative dose intensity—improving treatment and outcomes in early-stage breast cancer: a retrospective study. Oncol Nurs Forum. 2012;39(6):E459-467.
doi pubmed - Hershman DL, Unger JM, Barlow WE, Hutchins LF, Martino S, Osborne CK, Livingston RB, et al. Treatment quality and outcomes of African American versus white breast cancer patients: retrospective analysis of Southwest Oncology studies S8814/S8897. J Clin Oncol. 2009;27(13):2157-2162.
doi pubmed - Lee S, Kang DH, Ahn TS, Kim SS, Yun JH, Kim HJ, Seo SH, et al. The impact of pre-chemotherapy body composition and immunonutritional markers on chemotherapy adherence in stage III colorectal cancer patients. J Clin Med. 2023;12(4):1423.
doi pubmed - Jeong Y, Han HS, Lee HD, Yang J, Jeong J, Choi MK, Kwon J, et al. A pilot study evaluating steroid-induced diabetes after antiemetic dexamethasone therapy in chemotherapy-treated cancer patients. Cancer Res Treat. 2016;48(4):1429-1437.
doi pubmed - Lee EK, Koo B, Hwangbo Y, Lee YJ, Baek JY, Cha YJ, Kim SY, et al. Incidence and disease course of new-onset diabetes mellitus in breast and colorectal cancer patients undergoing chemotherapy: A prospective multicenter cohort study. Diabetes Res Clin Pract. 2021;174:108751.
doi pubmed - Hutajulu SH, Oktariani S, Sunggoro AJ, Bintoro BS, Astari YK, Wiranata JA, Widodo I, et al. The occurrence and risk factors of chemotherapy-induced neutropenia in patients with breast cancer not receiving primary G-CSF prophylaxis. Ecancermedicalscience. 2023;17:1618.
doi pubmed - Srokowski TP, Fang S, Hortobagyi GN, Giordano SH. Impact of diabetes mellitus on complications and outcomes of adjuvant chemotherapy in older patients with breast cancer. J Clin Oncol. 2009;27(13):2170-2176.
doi pubmed - Mashayekhi-Sardoo H, Mohammadpour AH, Nomani H, Sahebkar A. The effect of diabetes mellitus on pharmacokinetics, pharmacodynamics and adverse drug reactions of anticancer drugs. J Cell Physiol. 2019;234(11):19339-19351.
doi pubmed - Alenzi EO, Kelley GA. The association of hyperglycemia and diabetes mellitus and the risk of chemotherapy-induced neutropenia among cancer patients: A systematic review with meta-analysis. J Diabetes Complications. 2017;31(1):267-272.
doi pubmed - Yamaguchi K, Kusaba H, Makiyama A, Mitsugi K, Uchino K, Tamura S, Shibata Y, et al. The risk factors for oxaliplatin-induced peripheral sensory neuropathy and thrombocytopenia in advanced gastric cancer. Cancer Chemother Pharmacol. 2018;82(4):625-633.
doi pubmed - Klysiak M, Wieder-Huszla S, Branecka-Wozniak D, Karakiewicz-Krawczyk K, Napieracz-Trzosek I, Owsianowska J, Jurczak A, et al. Analysis of the occurrence of predicative factors of chronic fatigue in female patients with cancer of the reproductive organs with respect to stage of treatment. Int J Environ Res Public Health. 2023;20(4):3732.
doi pubmed - de Jesus Leite MAF, Puga GM, Arantes FJ, Oliveira CJF, Cunha LM, Bortolini MJS, Penha-Silva N. Effects of combined and resistance training on the inflammatory profile in breast cancer survivors: A systematic review. Complement Ther Med. 2018;36:73-81.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
World Journal of Oncology is published by Elmer Press Inc.