| World Journal of Oncology, ISSN 1920-4531 print, 1920-454X online, Open Access |
| Article copyright, the authors; Journal compilation copyright, World J Oncol and Elmer Press Inc |
| Journal website https://wjon.elmerpub.com |
Original Article
Volume 16, Number 5, October 2025, pages 525-529
A Comparison of Bidirectional Stratafix Continuous Suture Versus Conventional Interrupted Suture in Breast Mastectomy
Masanori Oshia, Akimitsu Yamadaa, b, c, Kei Kawashimaa, Mahato Sasamotoa, Itaru Endoa
aDepartment of Breast Surgery, Yokohama City University Graduate School of Medicine, Yokohama, Kanagawa 236-0004, Japan
bDepartment of Gastroenterological Surgery, Yokohama City University Graduate School of Medicine, Yokohama, Kanagawa 236-0004, Japan
cCorresponding Author: Akimitsu Yamada, Department of Gastroenterological Surgery, Yokohama City University Graduate School of Medicine, Yokohama, Kanagawa 236-0004, Japan
Manuscript submitted July 19, 2025, accepted August 30, 2025, published online September 17, 2025
Short title: Stratafix vs. Conventional Sutures in Mastectomy
doi: https://doi.org/10.14740/wjon2642
| Abstract | ▴Top |
Background: This study aimed to compare surgical outcomes between Stratafix barbed sutures and conventional sutures in patients undergoing total mastectomy for breast cancer.
Methods: This retrospective study analyzed patients who underwent total mastectomy and/or axillary lymph node dissection at our hospital.
Results: A total of 29 patients were included. No significant differences were observed in clinicopathological features between the two groups. However, the percentage of suturing time within the total operative time was significantly lower in the Stratafix group compared to conventional group (10% vs. 8%). In addition, the suturing time per centimeter was also significantly shorter with Stratafix group (P < 0.001). No wound-related complications were observed in either group during at least 3 months of follow-up.
Conclusions: The use of barbed sutures for wound closure in mastectomy procedures effectively reduces suturing time without increasing the incidence of wound complications. Bidirectional Stratafix barbed sutures offer an improved and efficient alternative to conventional sutures for breast surgeons.
Keywords: Suture; Breast cancer; Surgery; Surgical time
| Introduction | ▴Top |
Breast cancer is one of the most frequently diagnosed malignancies in women. Surgical treatment remains the gold standard, with the main options being breast conserving surgery (lumpectomy) and total mastectomy. Among these, total mastectomy accounts for approximately 40-80% of all breast cancer surgeries, with various depending on the country, patient age, and disease stage, and numerous procedures are performed globally each year. In many instances, multiple surgeries are conducted in a single day, and the duration of these operations can significantly impact not only the patients and breast surgeons but also the overall functioning of the hospital. In recent years, bidirectional barbed sutures have been increasingly utilized for wound closure in various surgical procedures. Barbed sutures are designed with anchors oriented in the opposite direction of the needle at regular intervals. These anchors provide tissue support, enabling knot-free continuous suturing for wound closure. The employment of barbed sutures for wound closure has been reported to reduce both wound closure time and overall operative time [1, 2]. While the efficacy and safety of barbed sutures have been validated in numerous types of surgeries across many countries [3, 4], there have been no comparable studies specifically focusing on the breast surgery in Japan. Consequently, this study aimed to evaluate and compare the surgical outcomes of bidirectional barbed sutures (STRATAFIX Spiral PDS Plus Bi-directional (ETHICON, Inc., Raritan, NJ, USA)) versus conventional sutures (4-0 PDS Plus (ETHICON, Inc., Raritan, NJ, USA)) in breast surgery.
| Materials and Methods | ▴Top |
This prospective study included 29 patients who underwent total mastectomy for breast cancer at our institution between April 2023 and October 2023. The patients were categorized into two groups based on the suturing method used: conventional group (C-group; n = 14), which used a conventional control suturing technique (4-0 PDS Plus (ETHICON, Inc., Raritan, NJ, USA)), and Stratafix group (S-group; n = 15), which utilized 4-0 STRATAFIX Spiral PDS Plus Bi-directional (ETHICON, Inc., Raritan, NJ, USA)) barbed sutures. The continuous suturing was performed in S-group, whereas single ligation was employed in C-group. This was a retrospective observational study of patients undergoing total mastectomy. The choice of suture method (Stratafix or conventional sutures) was determined intraoperatively at the discretion of the attending surgeon, without predefined clinical criteria. Therefore, this study was not designed as a randomized controlled trial. Postoperative wound complications were monitored for at least 30 days after surgery, and all patients were routinely followed in outpatient clinics for a minimum of 3 months. Since Stratafix is up to 20 cm long and unsuitable for long incisions, PDS is more commonly used. In both groups, wound closure was performed with a single layer of subcuticular sutures. In each case, two surgeons participated in the closure procedure simultaneously. In the S-group, this was facilitated by the bidirectional needle design of the barbed suture, while in the C-group, the same two-surgeon approach was applied to maintain consistency. Although the surgeon-assistant combinations were nearly identical across cases, a few procedures involved different surgeons. Data comparisons between the two groups were conducted using the Mann-Whitney U test. Statistical significance was determined by a P value of less than 0.05. R software was used to perform for all analysis in the study.
The primary outcome measures for this analysis included suturing time, and complications of wound (wound infection, cellulitis, and flap necrosis). All patients provided written informed consent for the total mastectomy procedure. Data collected from the hospital database comprised patient age, body mass index (BMI), operation time, surgical methods, and the American Joint Committee on Cancer (AJCC)-stage. These clinicopathological features of two groups are shown here (Supplemental Material 1, wjon.elmerpub.com).
Based on a two-sample t-test to detect a mean difference of 2.1 min in suturing time with a standard deviation of 0.6 min, six patients (three per group) were required for 80% power and eight patients (four per group) for 90% power at a two-side 5% significance level. The study included 14 and 15 patients per group, satisfying the statistical power requirements for the primary analysis.
This study was approved by the Institutional Review Board (Approval No. B200700008) and conducted in accordance with the tenets of the Declaration of Helsinki (1964) and its subsequent amendments.
| Results | ▴Top |
Using Stratafix for closure reduces the average suturing proportion of total operative time for mastectomy with sentinel lymph node biopsy procedures by approximately 19%
First, we focused on cases where total mastectomy with sentinel node biopsy (SNB) was performed (patients who underwent axillary lymph node dissection were excluded) and, in the analysis involving total operative time, examined the gross time required for wound closure to evaluate the proportion of overall closure time within the total operative time.
The number of patients who underwent total mastectomy with SNB was 10 in the S-group and seven in the C-group. The average total operative time for total mastectomy with SNB was 76.5 min for the S-group and 102 min (P = 0.14) (Fig. 1a) for the C-group, while the average time required for total wound closure was 7.2 min and 10.2 min, respectively. Due to the limitation that Stratafix measures only 20 cm in length and is thus unsuitable for closure of long incisions, PDS was preferentially used. Thus, C-group contains more patients with larger breast volume, and it takes longer operative time. To standardize the suturing time, we calculated the proportion of total closure time within the total operative time. The proportion of suturing time within the total operative time was 7.9% in the S-group and 9.8% in the C-group (Fig. 1b), corresponding to an absolute reduction of 2% and a relative reduction of approximately 19%. During at least 3 months of follow-up, no wound-related complications, such as infection or dehiscence were observed in either group.
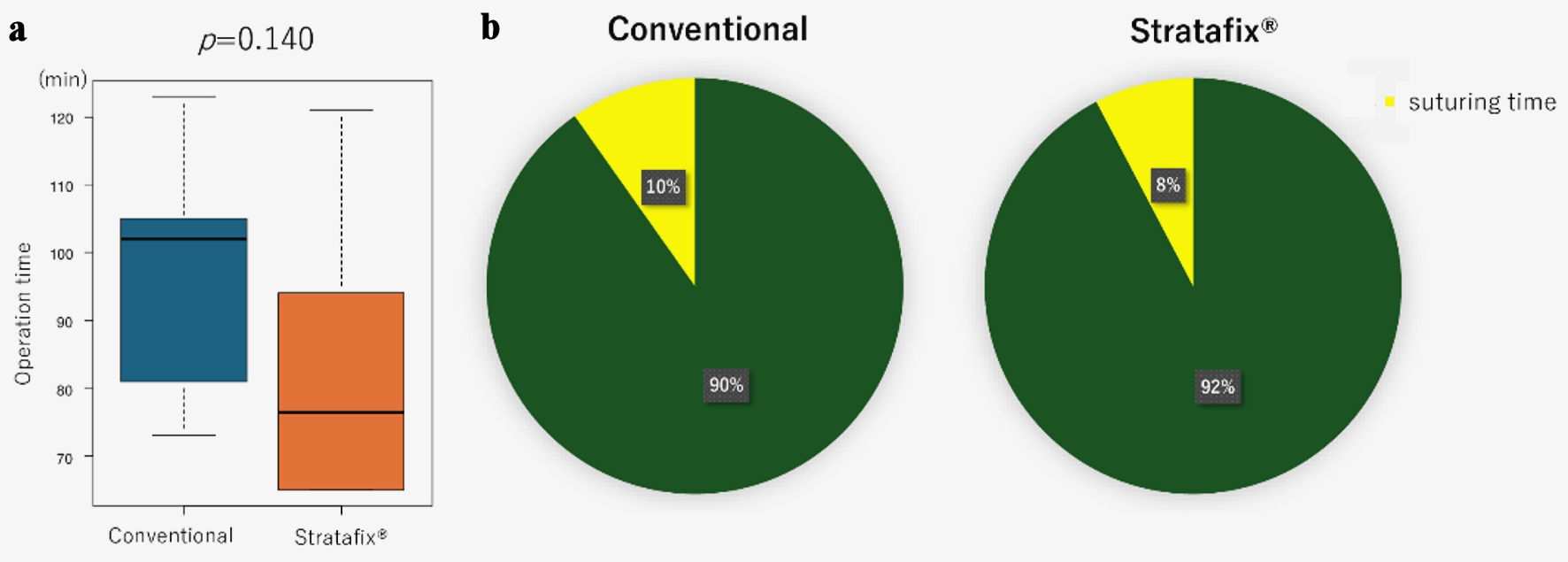 Click for large image | Figure 1. The difference of the time required for wound closure between C-group and S-group in cases undergoing total mastectomy with sentinel lymph node biopsy. (a) Boxplots showed a comparison of total operation time between C-group and S-group. The Mann-Whitney U test was used to calculate P value. (b) Pie chart showed the percentage of suturing time within the total operative time for each group. |
The time taken to close a 15-cm wound was significantly shorter in the S-group compared to the C-group
Considering that wound closing time varies depending on the wound length, we analyzed the closing time per 15 cm of wound length. We found that nearly all cases in the S-group had shorter closure times compared to any case in the C-group (Fig. 2a). The average time required to close a 15-cm wound was 5.9 min for S-group and 10.4 min for C-group, respectively, with the S-group showing 43% of reduction of suture time (Fig. 2b).
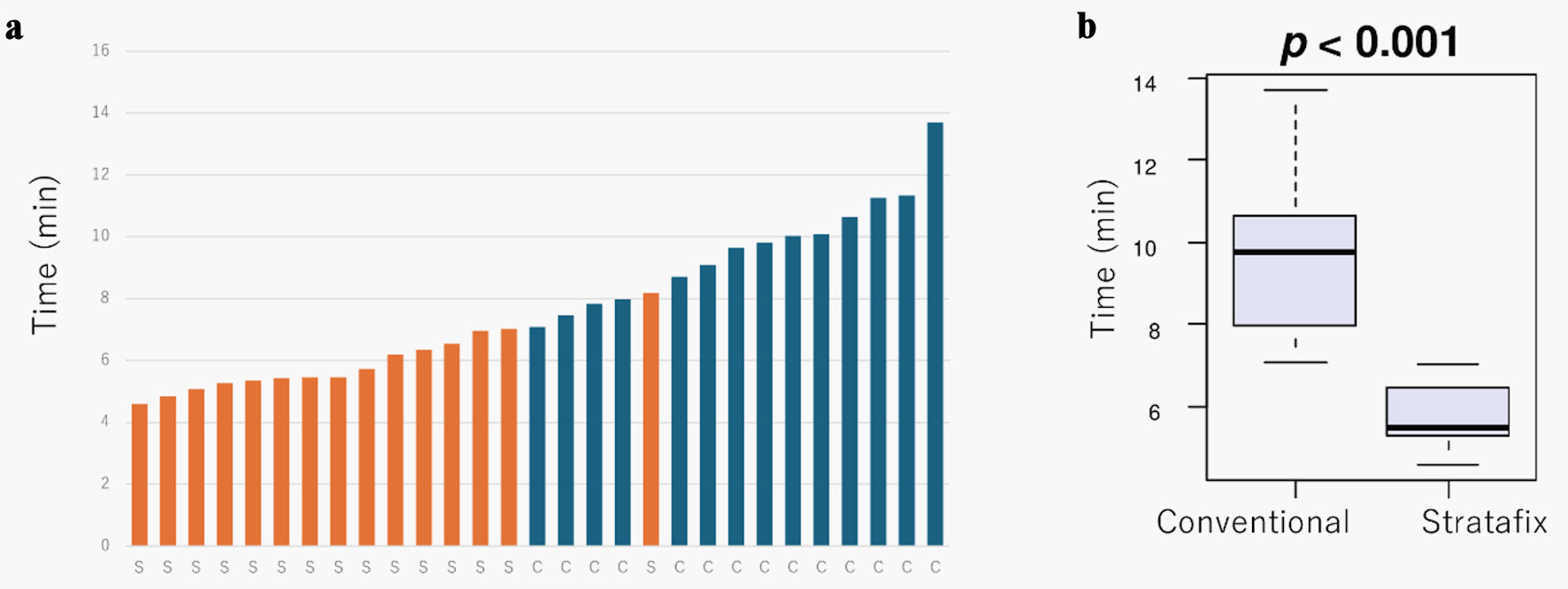 Click for large image | Figure 2. The difference in wound closure times of wound length between the C-group (blue) and S-group (orange). (a) Bar graph showing the time required for wound closure of 15 cm in each patient. (b) Boxplots of comparing the time required for 15-cm wound closure between the C-group and S-group. Mann-Whitney U test was used to calculate P value. |
The longer the wound length, the shorter the time required to close a 1-cm wound
Next, we examined how wound length influenced the closure time in both groups. We hypothesized that, due to continuous suturing in the S-group, the closure time would decrease as the wound length increased. Interestingly, not only in the S-group but also in the C-group, there was a tendency for the closure time per 1-cm wound to decrease as the total wound length increased (Fig. 3).
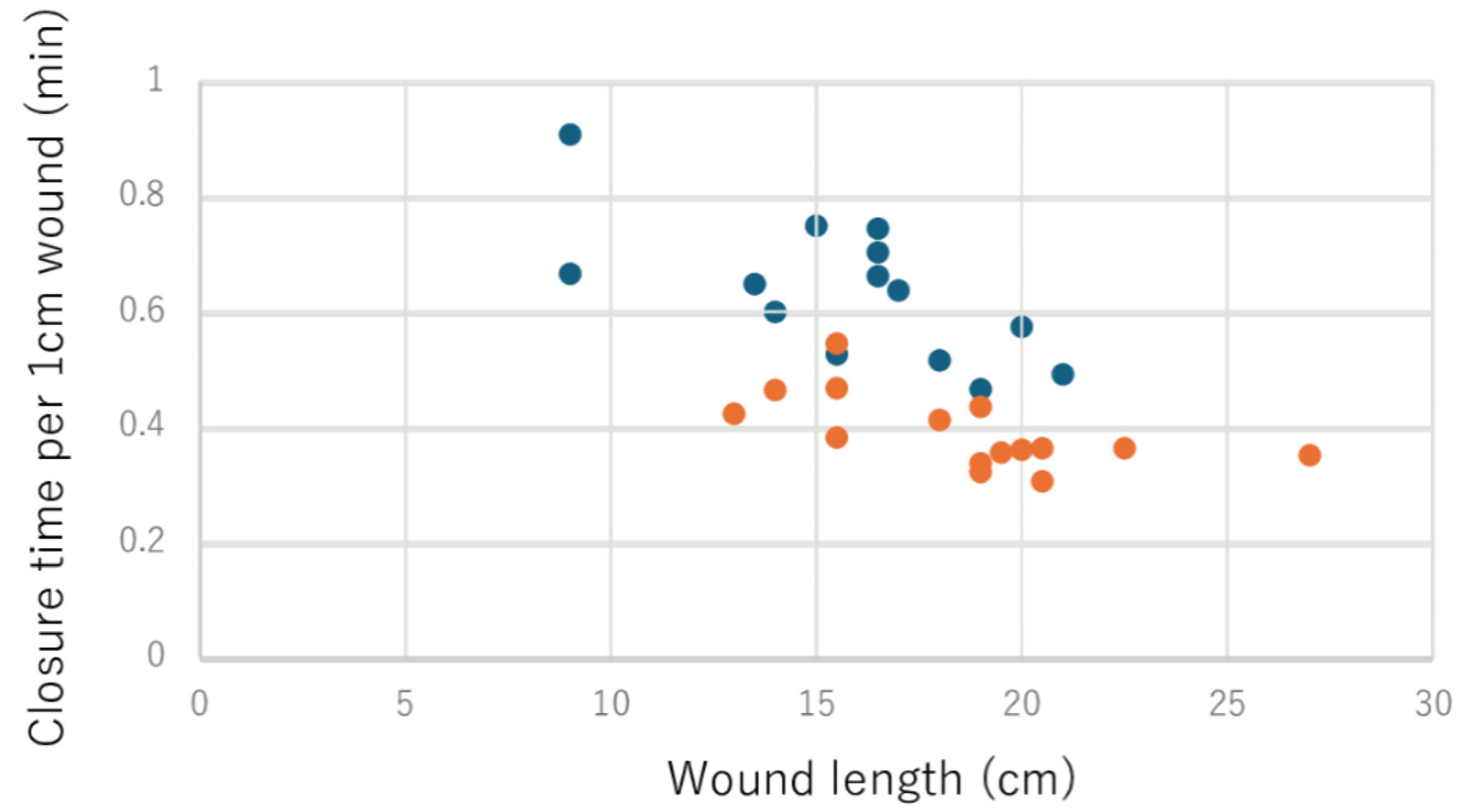 Click for large image | Figure 3. The relationship between wound length and closure time per 1-cm wound in both groups. Dot plots showed the correlation between actual wound length and wound closure time to 1-cm for each patient by C-group (blue) and S-group (orange). |
| Discussion | ▴Top |
In this study, we evaluated the efficacy of using barbed suture with Stratafix in breast surgery. The time required for wound closure per unit length was significantly shorter in the S-group. In the analysis limited to the cases of mastectomy with SNB procedure, the S-group showed a 43% reduction in suturing time.
Although the absolute reduction in operative time by employing barbed suture with Stratafix was approximately 2% for a single mastectomy with SNB procedure, this corresponds to a relative reduction of about 19% in the proportion of suturing time within the total surgery duration. Given that breast cancer surgeries are relatively shorter in duration compared to other cancer surgeries, this relative time saving may still be clinically meaningful.
Operative time tended to be shorter in the S-group in mastectomy with SNB procedure. This finding aligns with previous literature, whereas it represents the inaugural report within breast cancer surgery. One plausible explanation for the reduced operative time with barbed sutures is that the barbs allow the suture to remain securely anchored as it is tensioned, creating a stable fixation without the need for knot tying. This feature enables the surgeon to perform continuous suturing more efficiently, as the suture itself maintains tension throughout the process, eliminating the need for frequent adjustments and ensuring a more stable, consistent closure with fewer interruptions compared to traditional suturing techniques. Furthermore, the utilization of Stratafix barbed sutures, which do not necessitate knotting, mitigated the surgeon’s ligature-related stress. Although this effect is difficult to quantify, it facilitated a more comfortable closure process.
Interestingly, as the length of the incision increases, the suturing time per unit length becomes shorter. This can be explained by several factors. First, the relative impact of preparatory tasks such as needle adjustment and tension control becomes smaller as incision length increases, improving overall efficiency [5, 6]. Second, longer incisions allow surgeons to develop a steady rhythm through repetitive hand movements, leading to procedural optimization [7, 8]. Third, fixed-time tasks such as tension adjustments and knot-tying are spread over a greater distance, reducing their time burden per unit length. These findings suggest that procedural efficiency improves with longer incisions, even under consistent suture conditions [6].
Although postoperative wound healing was routinely followed up in outpatient clinics, a systemic evaluation and comparison of cosmetic outcomes between the groups was not conducted in this study. Therefore, aesthetic outcomes were not included as a formal endpoint. In addition, although all patients were followed for at least 3 months and no wound-related complications were observed in either group, the long-term follow-up was not sufficient. Hence, further evaluation focusing on cosmetic outcomes and wound healing over an extended period will be required. However, previous studies [9] have reported satisfactory cosmetic results without an increased risk of wound-related complications such as infection or dehiscence. These findings support the notion that barbed sutures can be acceptable from both functional and cosmetic perspectives, although comprehensive evaluation within breast surgery populations remains necessary.
The higher material cost associated with barbed sutures such as Stratafix must be weighed against the potential benefits of operative time reduction. Although this study did not perform a formal cost-effectiveness analysis, it should be noted that surgical costs are influenced not only by the price of sutures but also by factors such as operating room time and personnel expenses. Therefore, a comprehensive economic evaluation is necessary to fully understand the cost-benefit balance. Future research should explore whether the savings in operative time and surgeon workload justify the additional material expenses in breast surgery.
In addition to the observed reduction in operative time, all surgeons involved in this study subjectively reported a smoother suturing experience when using Stratafix compared to conventional suturing techniques. Although surgeon satisfaction was not formally assessed through structured questionnaires or scoring systems, the perceived improvement in workflow and reduction in operative stress were consistently noted across all operators. These anecdotal observations suggest that barbed sutures may not only benefit patients by reducing surgical time but also contribute positively to the surgical team’s intraoperative experience. Future studies could formally assess surgeon-reported outcomes to further quantify this potential benefit.
This study is subject to certain limitations. First, selection bias may have been introduced. As previously described, because Stratafix sutures are limited to a length of 20 cm and are therefore unsuitable for closure of longer incisions, PDS sutures were preferentially used for patients with larger breast volumes and longer excision wounds. This could have influenced the wound closure times independently of the suture material itself. Second, the relatively small sample size increases the potential influence of outliner cases on the average closure times, limiting the generalizability of the findings. Third, the advantage of continuous suturing techniques, such as Stratafix, may become more apparent in cases with longer incision lengths; thus, the observed benefits might not fully extrapolate to shorter incisions. Therefore, additional investigations with larger cohort and randomized controlled trial designs are warranted to validate and extend these findings.
Conclusions
Stratafix, a bidirectional barbed suture, has been shown to substantially reduce both surgical and suturing durations in mastectomy procedures. These bidirectional barbed sutures offer simplicity in application and serve as an efficient technique for breast cancer surgery.
| Supplementary Material | ▴Top |
Suppl 1. Background of characteristics of patients in the study.
Acknowledgments
None to declare.
Financial Disclosure
This research was supported by Grants-in-Aid for Scientific Research from the Japan Society for the Promotion of Science, JSPS grant number 21K15535 to AY, and 23K14600 to MO.
Conflict of Interest
AY received honoraria from AstraZeneca, Chugai Pharmaceutical, Daiichi Sankyo, Eisai, Eli Lily, Kyowa Kirin, Medicon, MSD, Pfizer, Takeda pharmaceutical, and Taiho outside the submitted work. All remaining authors have no competing interests to declare.
Informed Consent
Informed consent was obtained from all patients.
Author Contributions
MO researched the literature and wrote the manuscript. KK, MS, AY, and IE contributed to the pathological diagnosis of the patient. AY, and IE contributed to the manuscript review. All authors read and approved of the final manuscript.
Data Availability
Any inquiries regarding supporting data availability of this study should be directed to the corresponding author.
| References | ▴Top |
- Shi K, Chen X, Shen B, Luo Y, Lin R, Huang Y. The use of novel knotless barbed sutures in posterior long-segment lumbar surgery: a randomized controlled trial. J Orthop Surg Res. 2022;17(1):279.
doi pubmed - Mun J, Hyun SJ, Lee JK, An S, Kim KJ. Surgical and clinical outcomes associated with the use of barbed sutures and self-adhering mesh system and polymeric glue for wound closure in multilevel or revision spinal surgery: a matched cohort comparative study with conventional wound closure procedure. Neurospine. 2023;20(3):981-988.
doi pubmed - Cortez R, Lazcano E, Miller T, Hein RE, Constantine RS, Anigian K, Davis KE, et al. Barbed sutures and wound complications in plastic surgery: an analysis of outcomes. Aesthet Surg J. 2015;35(2):178-188.
doi pubmed - Salzberg CA. Barbed sutures in breast reconstruction. Aesthet Surg J. 2013;33(3 Suppl):40S-43S.
doi pubmed - Borner G, Montgomery A. Suture-tool: a mechanical needle driver for standardized wound closure. World J Surg. 2020;44(1):95-99.
doi pubmed - Klonner ME, Degasperi B, Bockstahler B, Dupre G. Suture length to wound length ratio for simple continuous abdominal closures in veterinary surgery: An experimental in vitro study. PLoS One. 2019;14(4):e0215641.
doi pubmed - Gilat R, Haunschild ED, Tauro T, Parvaresh KC, Cole BJ. Time to closure of orthopaedic surgical incisions: a novel skin closure device versus conventional sutures. J Wound Care. 2021;30(2):130-133.
doi pubmed - Song M, Cho Y. A prospective randomized controlled study of stratafix versus standard-of-care for deep tissue closure in orthopedic surgery. Clin Orthop Surg. 2024;16(5):820-826.
doi pubmed - Msallam EAM, Alam B, Akram T, Akbari AR. Reviewing the efficacy, safety and aesthetic outcome of barbed suture use in neck dissection. Eur Arch Otorhinolaryngol. 2025;282(6):3387.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
World Journal of Oncology is published by Elmer Press Inc.