| World Journal of Oncology, ISSN 1920-4531 print, 1920-454X online, Open Access |
| Article copyright, the authors; Journal compilation copyright, World J Oncol and Elmer Press Inc |
| Journal website https://wjon.elmerpub.com |
Original Article
Volume 16, Number 5, October 2025, pages 478-486
Predictors of All-Cause In-Hospital Mortality in Patients With Malignant Well-Differentiated Gastroenteropancreatic Neuroendocrine Tumors
Elvis Obomanua, b, d, Tarfa Verinumbea, Tinsae Aneboa, Colton Jonesa, Claudia Douradoc
aDepartment of Internal Medicine, Jefferson Einstein Hospital, Philadelphia, PA, USA
bSydney Kimmel Medical College, Thomas Jefferson University, Philadelphia, PA, USA
cDepartment of Hematology-Oncology, Jefferson Einstein Hospital, Philadelphia, PA, USA
dCorresponding Author: Elvis Obomanu, Department of Internal Medicine, Jefferson Einstein Hospital, Philadelphia, PA 19141, USA
Manuscript submitted May 27, 2025, accepted August 9, 2025, published online September 17, 2025
Short title: In-Hospital Mortality in Malignant WD GEP-NETs
doi: https://doi.org/10.14740/wjon2614
| Abstract | ▴Top |
Background: Factors influencing in-hospital mortality in patients with well-differentiated gastroenteropancreatic neuroendocrine tumors (GEP-NETs) remain understudied, highlighting gaps in optimizing acute clinical outcomes. This study aimed to identify sociodemographic and clinical predictors of all-cause in-hospital mortality in this population.
Methods: Using 2016 - 2020 data from the National Inpatient Sample (NIS), patients with malignant well-differentiated GEP-NETs were identified via the International Classification of Diseases, 10th Revision (ICD-10) codes. The primary outcome was in-hospital mortality. Sociodemographic and clinical variables (heart failure (HF), malnutrition, Charlson Comorbidity Index (CCI), and tumor site) were analyzed using multivariable logistic regression.
Results: Among 5,642 patients (mean age 64, standard deviation (SD) 12.9), multivariable analysis identified HF (adjusted odds ratio (aOR) 2.09, 95% confidence interval (CI): 1.10 - 3.95), malnutrition (aOR 1.84, 95% CI: 1.29 - 2.62), pancreatic (aOR 1.52, 95% CI: 1.01 - 2.30) or colon tumors (aOR 2.31, 95% CI: 1.51 - 3.53), CCI ≥ 5 (aOR 1.49, 95% CI: 1.06 - 2.10), hypertension (aOR 0.65, 95% CI: 0.47 - 0.91) and elective admissions (aOR 0.40, 95% CI: 0.25 - 0.63) as clinically relevant factors associated with in-hospital mortality.
Conclusions: Advanced age, tumor location, malnutrition, and HF may be critical mortality predictors among patients with GEP-NETs. These findings advocate for integrated care models prioritizing nutritional support, cardiovascular monitoring, and early elective interventions to improve outcomes.
Keywords: Gastroenteropancreatic neuroendocrine tumors; Malignant well-differentiated tumors; All-cause mortality; In-hospital mortality
| Introduction | ▴Top |
Gastroenteropancreatic neuroendocrine tumors (GEP-NETs) comprise a heterogeneous group of neoplasms originating from the neuroendocrine system of the gastrointestinal (GI) tract and pancreas. They exhibit diverse clinical behavior and prognosis. The incidence of GEP-NETs has increased substantially in recent decades, with estimates in the United States ranging from 3.8 to 6.5 cases per 100,000 individuals annually [1, 2]. Advances in diagnostic imaging and endoscopic techniques have contributed to this rising incidence. Despite their classification of some of these tumors as well-differentiated, they possess the capacity for aggressive behavior, including hepatic metastasis and secretion of bioactive peptides that precipitate debilitating paraneoplastic syndromes [3-5].
Despite extensive research on long-term outcomes, factors influencing in-hospital mortality, a critical endpoint reflecting acute clinical deterioration, remain poorly characterized in this population. Existing studies highlight the prognostic role of tumor biology, treatment modalities, and long-term survival, leaving a gap in understanding the determinants of acute mortality in hospitalized patients [6-10]. This gap is particularly consequential given the rising prevalence of well-differentiated GEP-NETs and the resource-intensive nature of their management [11, 12]. Emerging evidence suggests that non-oncological factors like comorbid conditions may significantly influence short-term outcomes [13, 14]. However, these associations remain understudied and inconsistently reported. Identifying key clinical and sociodemographic factors that drive all-cause mortality in these populations is essential, as these patient-centered variables interact with tumor biology to shape hospitalization outcomes.
This study aims to bridge the knowledge gap by leveraging a large-scale, nationally representative database to analyze the sociodemographic and clinical determinants of all-cause in-hospital mortality in patients with malignant well-differentiated GEP-NETs. Our study aims to provide actionable insights for refining risk stratification protocols and optimizing inpatient care, ultimately informing targeted interventions to reduce acute mortality in this population.
| Materials and Methods | ▴Top |
Data source and study sample
We analyzed secondary data from the 2016 - 2020 National Inpatient Sample (NIS), Healthcare Cost and Utilization Project (HCUP) database, the largest publicly available all-payer inpatient database in the USA. For this study, we analyzed data on patients admitted with malignant well-differentiated GEP-NETs from January 2016 to December 2020 in the USA. International Classification of Diseases, 10th Revision (ICD-10) codes for GEP-NETs (C25.4 and C7A.X) were used to determine our study sample. The following ICD codes were excluded from our study sample: C7A.090, C7A.091, C7A.093, C7A.098, C7A.8, C7A.1, as the tumors represented by these codes are beyond the scope of this study. These ICD-10 codes were excluded because they correspond to either diagnoses of poorly differentiated tumors or tumors that affected other non-GI sites, such as the lungs and bronchus. We also excluded C7A.020 which represented NET of the appendix because these tumors are usually incidental findings and may differ biologically and clinically from NETs at other sites. Due to the nature of administrative coding, our definition of “malignant” is limited to diagnoses explicitly coded as such. We recognize that certain NETs -such as functional pancreatic or duodenal NETs - may possess malignant potential but are not always coded accordingly, which may lead to underestimation of the true malignant GEP-NET population.
Measures
Outcome
The primary outcome assessed in this study was all-cause in-hospital mortality, which was dichotomized based on the patient’s final disposition on discharge.
Exposures
We assessed sociodemographic characteristics, including age at admission, sex (male, female), race and ethnicity (White, Black, Hispanic, and others), insurance status (private, Medicaid, Medicare, and others), and median household income national quartile for patient ZIP code.
Clinical characteristics that may contribute to in-hospital mortality were determined based on ICD diagnosis codes on the patient’s record. We included a history of essential hypertension (I10), heart failure with reduced ejection fraction (HFrEF, I50.2X), lower GI bleeding (K92.1, K92.2, and K62.5), protein energy malnutrition (PEM, E43.X, E44.X, E45.X, E46.X), obesity (E66.X, excluding E66.3), type 2 diabetes mellitus (DM, E11.65), iron deficiency anemia (D50.9), hyperlipidemia (E78.5) and lipid disorders (E78.X).
Our analysis included length of hospital stay, total hospital charges, survey year, type of hospital admission (elective vs. non-elective), and tumor site (appendix, small intestine, pancreas, rectum, colon, and stomach). We used the Charlson Comorbidity Index (CCI) to account for the comorbidities in the patients’ records at discharge. The CCI is a method of categorizing the severity of comorbidities based on a list of specific ICD-10 codes that identify 17 distinct comorbid conditions. We used the “charlson.ado” program in Stata to get a CCI score for each patient. The CCI is scored from 0 to 37, which we categorized as < 5 and ≥ 5 for this analysis. These thresholds were chosen based on a prior study by Huang et al [15], where the severity of comorbidity was categorized as mild (1 - 2), moderate (3 - 4), and severe (≥ 5). However, in our analysis, we decided to dichotomize the CCI scores as mentioned above due to sample size limitations and ease of interpretation.
Statistical analysis
Descriptive statistics were used to summarize our study sample’s sociodemographic and clinical characteristics, including frequencies and proportions. We used Pearson’s Chi-square and Fisher’s exact test to assess the differences in categorical variables between study participants who died and those who did not. Differences in continuous variables between the two groups were evaluated using the Student’s t-test. A multivariable logistic regression was used to determine the association between the above sociodemographic and clinical characteristics and all-cause in-hospital mortality. We used multivariable logistic regression to ensure the final model accounted for factors that could confound our relationship. Model fitness was determined using the Hosmer Lemeshow Goodness of Fit test. Estimates of the association between the variables, as mentioned earlier, and in-hospital mortality were presented as odds ratios and 95% confidence intervals (CIs). All analyses were performed using Stata version 18.0 (StataCorp LLC, College Station, TX, USA).
Ethics/Institutional Review Board (IRB) approval statement
IRB approval is not required for this study. The data are publicly available and were used in accordance with applicable data use agreement. All data and materials support the published claims and comply with field standards.
| Results | ▴Top |
Sociodemographic characteristics of the study sample
There were 5,642 patients admitted with malignant well-differentiated GEP-NETs who met the inclusion criteria. Of these, 22.0% were admitted in 2016, 21.6% in 2017, 20.7% in 2018, 20.1% in 2019 and 15.6% in 2020. The majority (70.7%) of participants identified as White, 51.3% were male, and the mean age was 64 years (standard deviation (SD) = 12.9 years). Most (53%) of the participants were insured through Medicare, while 35% had private insurance. Most (60.4%) hospitalizations were non-elective admissions, and participants had an average length of stay of 6.7 days (SD = 7.6). The mean hospital charge during hospitalization was $83,399 (SD = $154,359). A quarter (25%) of participants were in the second and fourth national income quartiles, based on median household income (Table 1).
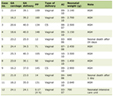 Click to view | Table 1. Sociodemographic Characteristics of Study Participants |
Common sites affected by GEP-NETs include small intestine (61%), pancreas (16%), colon (10%) and stomach (9%). Most participants (71%) had a CCI score of < 5. Comorbid conditions reported among participants in the study sample include obesity (15.0%), hyperlipidemia (27.7%), lipid disorders (34.0%), essential hypertension (43.9%), type 2 DM with hyperglycemia (4.6%), lower GI bleeding (2.6%), PEM (15.6%), HFrEF (2.5%) and iron deficiency anemia (4.1%).
Overall, 195 (3.2%) patients with GEP-NETs from 2016 - 2020 died during hospital admission.
Factors associated with in-hospital mortality among patients with GEP-NETs
In unadjusted analyses, sociodemographic characteristics associated with in-hospital mortality were age (odds ratio (OR) 1.03, 95% CI: 1.02 - 1.04) and insurance type. Clinical characteristics associated with in-hospital mortality were obesity (OR 0.59, 95% CI: 0.36 - 0.96), hyperlipidemia (OR 0.62, 95% CI: 0.44 - 0.89), lipid disorders (OR 0.61, 95% CI: 0.43 - 0.84), essential hypertension (OR 0.54, 95% CI: 0.40 - 0.74), HFrEF (OR 3.46, 95% CI: 1.99 - 6.03) and PEM (OR 3.06, 95% CI: 2.26 - 4.15). Our study showed that patients on elective admissions had a lower mortality risk (OR 0.25, 95% CI: 0.17 - 0.37) than non-elective admissions patients. Participants with tumors located at the pancreas (OR 2.10, 95% CI: 1.47 - 2.99), and colon (OR 2.30, 95% CI: 1.54 - 3.45) had a significantly higher risk of mortality compared to those with tumors at the small intestine. In addition, participants with more extended hospital stays had a statistically significant higher risk of in-hospital mortality (OR 1.03, 95% CI: 1.01 - 1.06). Lastly, a CCI score of ≥ 5 was associated with two times higher odds of in-hospital mortality (OR 2.15, 95% CI: 1.61 - 2.87) (Table 2).
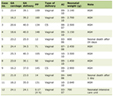 Click to view | Table 2. Factors Associated With Mortality Among Patients Admitted With GEP-NETs |
Adjusted multivariable logistic regression showed that age was the only sociodemographic characteristic that was statistically associated with in-hospital mortality (adjusted odds ratio (aOR) 1.03, 95% CI: 1.02 - 1.05), although our results suggest that this association may not be clinically significant. Our study found a diagnosis of HFrEF (aOR 2.09, 95% CI: 1.10 - 3.95), PEM (aOR 1.84, 95% CI: 1.29 - 2.62), and essential hypertension (aOR 0.65, 95% CI: 0.47 - 0.91) were significantly associated with in-hospital mortality. Participants on elective admissions had a lower mortality risk than those on non-elective admissions (aOR 0.40, 95% CI: 0.25 - 0.63). Participants with tumors located at the pancreas (aOR 1.52, 95% CI: 1.01 - 2.30) and colon (aOR 2.31, 95% CI: 1.51 - 3.53) had a significantly higher risk of mortality compared to those with tumors in the small intestine. Finally, participants with a CCI score of ≥ 5 had a significantly increased risk of in-hospital mortality compared to those with a lower index score (aOR 1.49, 95% CI: 1.06 - 2.10). The results of the association of all the other factors assessed and in-hospital mortality were inconclusive (Table 2).
| Discussion | ▴Top |
This study demonstrates that patient-specific factors, including comorbidities, tumor location, and type of admission, significantly influence outcomes in patients with malignant well-differentiated GEP-NETs. Our analysis identified HFrEF, PEM, pancreatic and colonic tumor locations, and a high CCI (≥ 5) as independent factors associated with increased risk of in-hospital mortality. While older age was identified as a statistically significant factor associated with mortality, our findings show that this finding may not be clinically significant. Conversely, hypertension and elective hospitalization were associated with reduced risk of in-hospital mortality. Notably, our findings confirm the overall favorable prognosis of well-differentiated GEP-NETs, with a 5-year mortality rate of 3.2%, consistent with studies showing good overall survival in this population [8, 16].
Previous studies have identified advanced age as a predictor of in-hospital mortality in patients with well-differentiated tumors, independent of tumor biology [8, 14, 17, 18]. The immunological consequences of aging, including decreased immunosurveillance and increased immune senescence, contribute to tumor progression and poorer outcomes [19-21]. Frailty, a hallmark of aging, is associated with diminished physiological reserve, poor cancer outcomes, and reduced tolerance to curative therapies, such as surgery and aggressive chemotherapy [22-26]. Older adults may also be more likely to forgo aggressive treatments in favor of palliative care due to various health and sociodemographic factors [27, 28]. Furthermore, the increased comorbidities associated with age can alter the tumor microenvironment, compromise cancer therapy response, and ultimately reduce survival [29, 30]. Consistent with our findings, older patients and those with a high CCI (> 5) were at increased risk of in-hospital mortality, although in our cohort, the effect of age, while statistically significant, appeared to be of limited clinical relevance. To improve outcomes, older patients with these tumors would benefit from comprehensive geriatric assessments, optimization of comorbidities, and rehabilitation strategies.
Despite their well-differentiated classification, pancreatic and colonic well-differentiated GEP-NETs exhibit distinct biological and clinical risks. Colonic well-differentiated NETs are often diagnosed at an advanced stage, with widespread metastasis to the liver, nodes, and mesentery [31]. In pancreatic well-differentiated NETs, mutations in genes such as MEN1, DAXX, ATRX, and MTOR are associated with aggressive behavior, metastasis, genomic instability, therapy resistance, and reduced overall survival [32-35]. These tumors exhibit increased variability in Ki-67 scores, suggesting potential aggressiveness despite their well-differentiated morphology. [36, 37]. Furthermore, functional pancreatic NETs, especially those associated with insulinomas and VIPoma, are associated with poorer outcomes [38]. Complex tumor anatomies, such as those located in the pancreatic head, can render curative surgical therapies infeasible, leading to worse survival outcomes [39, 40]. Although the PROMID trial [41] and CLARINET trial [42] established the efficacy of somatostatin analogs for GEP-NETs, epigenetic modifications in well-differentiated GEP-NETs can confer resistance to these therapies, resulting in poor outcomes [43]. Prioritizing early detection and site-specific monitoring may improve outcomes in this population.
Optimal nutrition modulates immune function, enhances immune surveillance, and prevents tumor progression [44, 45]. Unfortunately, malnutrition is a prevalent issue in cancer patients, affecting 20-70% of patients depending on the cancer type, disease stage, and clinical setting [46]. Patients with GEP-NETs exhibit a malnutrition prevalence of approximately 25% [47]. Malnutrition compromises tolerance to chemotherapy, leading to increased toxicity, reduced compliance, and diminished treatment efficacy, ultimately resulting in heightened tumor aggressiveness and mortality [48]. Furthermore, malnourished cancer patients experience poor surgical outcomes, hindering postoperative recovery and increasing mortality risk [49, 50]. In the context of functional GEP-NETs, malnutrition is exacerbated by catabolic states, diarrhea, and worsening nutritional status, ultimately impacting tumor aggressiveness and overall survival [51]. Our findings suggest that PEM is a critical predictor of in-hospital mortality in patients with well-differentiated GEP-NETs. These results underscore the imperative for timely and integrated nutritional interventions to mitigate malnutrition-related complications and optimize health-related quality-of-life outcomes in this population.
HFrEF is a prevalent and prognostically significant comorbidity in patients with well-differentiated GEP-NET, affecting approximately 50% of this population [13]. The relationship between well-differentiated GEP-NETs and HFrEF is bidirectional, with carcinoid heart disease potentially contributing to the development of HFrEF through the deposition of vasoactive substances on the heart [52]. In our study, there was a 2.28-fold increased risk of mortality in patients with well-differentiated GEP-NETs and comorbid HFrEF, aligning with observational data demonstrating elevated mortality in cancer patients with heart failure compared to the general population [53]. Conversely, cancer is a leading cause of non-cardiovascular death in patients with heart failure [54]. The introduction of novel therapies, such as tyrosine kinase inhibitors (TKIs), which have improved progression-free survival in well-differentiated GEP-NETs, may be limited in their use due to their potential cardiovascular side effects, which may exacerbate heart failure and worsen outcomes [55]. Therefore, vigilant cardiovascular monitoring and timely therapeutic intervention are crucial to mitigating the adverse prognostic implications of heart failure in well-differentiated GEP-NETs.
Timely healthcare-seeking is essential for optimizing cancer survival outcomes. An Australian study demonstrated that cancer patients admitted through emergency departments had a four-fold increased likelihood of mortality within 12 months compared to those with elective admissions. [56]. This finding is corroborated by other studies highlighting the association between emergency admissions and increased mortality [57, 58]. Our study’s observation of reduced in-hospital mortality among patients with elective admissions may be attributed to better preparation, timely interventions, and potentially less advanced disease progression. Notably, our analysis revealed a statistically significant association between hypertension and decreased mortality, contrasting with existing literature linking hypertension to increased cancer-related deaths [59, 60]. A potential explanation for this unexpected finding is that hypertension may enhance tumor blood flow, facilitate chemotherapy delivery and reduce hypoxia-induced chemoresistance. The relationship between hypertension and cancer outcomes is influenced by factors such as cancer type, stage, and hypertension severity. The observed association between essential hypertension and reduced mortality risk in this cancer subtype warrants further exploration to elucidate underlying biological mechanisms.
Additional hospital-related factors, including obesity, DM, GI bleeding, length of hospital stay, and hyperlipidemia, were evaluated for their potential association with mortality outcomes. However, our analysis yielded inconclusive results, suggesting that these factors may not significantly impact mortality.
This study has some limitations that warrant consideration. First, its cross-sectional design precludes the establishment of temporality, and the findings should be interpreted as correlational rather than causal. Second, the reliance on claims data from the NIS database, which utilizes ICD-9 and ICD-10 codes for diagnosis confirmation, introduces potential biases inherent to retrospective claim-based research. Accurate identification of GEP-NETs may be compromised by misclassification or underreporting. For example, functional pancreatic NETs and duodenal NETs are sometimes miscoded as benign, despite their malignant potential. As a result, our reliance on diagnostic codes may underestimate the true burden of disease. While we defined “malignant” NETs based on available ICD-10 codes, we acknowledge that this may not fully capture the complexity and heterogeneity of GEP-NET classification. Third, the NIS dataset lacks granular clinical information, including tumor stage, histologic grade, functional status, and other clinicopathologic features that are critical for prognostication and treatment decision-making in patients with GEP-NETs. Consequently, our ability to adjust for disease severity or stratify outcomes by stage was limited. Fourth, although surgical intervention is a cornerstone of NET management and can be associated with both favorable and unfavorable outcomes depending on timing and indication, we were unable to analyze surgical procedures due to the lack of specificity in procedure coding. The NIS does not reliably distinguish between curative resections, palliative surgeries, or unrelated operations. Furthermore, surgical intervention may be associated with improved survival when tumors are detected early and completely resected, but this nuance could not be captured in our analysis. Fifth, the NIS dataset’s structure, which records readmissions as distinct observations, precluded the analysis of readmission rates. Although our sample size was substantial, a larger cohort may have yielded more statistically significant results for certain variables. Finally, while demographic factors were adjusted for in the analysis, residual confounding variables may still influence the findings. Future studies utilizing clinical registries or datasets with more detailed oncologic variables are needed to better characterize mortality drivers and inform care in this rare population.
Conclusions
This study highlights the complex interplay of factors contributing to increased mortality in patients with malignant well-differentiated GEP-NET. Advanced age, tumor location in the colon and rectum, PEM, and heart failure are significant predictors of poor outcomes in this population. These results underscore the importance of a multidisciplinary approach to patient care, incorporating timely nutritional interventions, optimal tumor management, and careful monitoring for cardiovascular complications. These findings emphasize the importance of integrating these variables into prognostic models, which can facilitate risk stratification and inform clinical decision-making for hospitalized patients with malignant well-differentiated GEP-NETs.
Acknowledgments
This study used data from the NIS, a publicly available database sponsored by the Agency for Healthcare Research and Quality (AHRQ) and its partners (https://hcup-us.ahrq.gov/db/hcupdatapartners.jsp) as part of the Healthcare Cost and Utilization Project (HCUP). The authors are solely responsible for the design and conduct of the study, the analysis and interpretation of the data, and the preparation of the manuscript. The views expressed in this article do not necessarily reflect those of AHRQ or HCUP.
Financial Disclosure
Publication made possible in part by support from the Thomas Jefferson University Open Access Fund.
Conflict of Interest
All the authors declare no conflict of interest.
Informed Consent
Formal consent is not required for this study.
Author Contributions
EO: conceptualization, writing - original draft, writing - review and editing. TV: methodology, data curation, formal analysis, writing - original draft, writing - review and editing. TA: writing - review and editing. CJ: writing - review and editing. CD: writing - review and editing.
Data Availability
The data underlying this study’s findings are available from the author upon reasonable request.
| References | ▴Top |
- Lee MR, Harris C, Baeg KJ, Aronson A, Wisnivesky JP, Kim MK. Incidence trends of gastroenteropancreatic neuroendocrine tumors in the United States. Clin Gastroenterol Hepatol. 2019;17(11):2212-2217.e2211.
doi pubmed - Takayanagi D, Cho H, Machida E, Kawamura A, Takashima A, Wada S, Tsunoda T, et al. Update on epidemiology, diagnosis, and biomarkers in gastroenteropancreatic neuroendocrine neoplasms. Cancers (Basel). 2022;14(5).
doi pubmed - Sansone A, Lauretta R, Vottari S, Chiefari A, Barnabei A, Romanelli F, Appetecchia M. Specific and non-specific biomarkers in neuroendocrine gastroenteropancreatic tumors. Cancers (Basel). 2019;11(8):1113.
doi pubmed - Cives M, Strosberg JR. Gastroenteropancreatic neuroendocrine tumors. CA Cancer J Clin. 2018;68(6):471-487.
doi pubmed - Fernandez CJ, Agarwal M, Pottakkat B, Haroon NN, George AS, Pappachan JM. Gastroenteropancreatic neuroendocrine neoplasms: A clinical snapshot. World J Gastrointest Surg. 2021;13(3):231-255.
doi pubmed - Chauhan A, Chan K, Halfdanarson TR, Bellizzi AM, Rindi G, O'Toole D, Ge PS, et al. Critical updates in neuroendocrine tumors: Version 9 American Joint Committee on Cancer staging system for gastroenteropancreatic neuroendocrine tumors. CA Cancer J Clin. 2024;74(4):359-367.
doi pubmed - Del Rivero J, Perez K, Kennedy EB, Mittra ES, Vijayvergia N, Arshad J, Basu S, et al. Systemic therapy for tumor control in metastatic well-differentiated gastroenteropancreatic neuroendocrine tumors: ASCO guideline. J Clin Oncol. 2023;41(32):5049-5067.
doi pubmed - Xu Z, Wang L, Dai S, Chen M, Li F, Sun J, Luo F. Epidemiologic trends of and factors associated with overall survival for patients with gastroenteropancreatic neuroendocrine tumors in the United States. JAMA Netw Open. 2021;4(9):e2124750.
doi pubmed - Sedlack AJH, Varghese DG, Naimian A, Yazdian Anari P, Bodei L, Hallet J, Riechelmann RP, et al. Update in the management of gastroenteropancreatic neuroendocrine tumors. Cancer. 2024;130(18):3090-3105.
doi pubmed - Tang LH, Untch BR, Reidy DL, O'Reilly E, Dhall D, Jih L, Basturk O, et al. Well-differentiated neuroendocrine tumors with a morphologically apparent high-grade component: a pathway distinct from poorly differentiated neuroendocrine carcinomas. Clin Cancer Res. 2016;22(4):1011-1017.
doi pubmed - Grande E, Diaz A, Lopez C, Munarriz J, Reina JJ, Vera R, Bernardez B, et al. Economics of gastroenteropancreatic neuroendocrine tumors: a systematic review. Ther Adv Endocrinol Metab. 2019;10:2042018819828217.
doi pubmed - Laskaratos FM, Caplin M. Treatment challenges in and outside a network setting: Gastrointestinal neuroendocrine tumours. Eur J Surg Oncol. 2019;45(1):52-59.
doi pubmed - Algeri L, Falkman L, Spada F, Frassoni S, Bagnardi V, Boselli S, Cardinale D, et al. Carcinoid heart disease in patients with advanced small-intestinal neuroendocrine tumors and carcinoid syndrome: a retrospective experience from two European referral centers. ESMO Open. 2024;9(11):103959.
doi pubmed - Keller HR, Senapathi SH, Morada A, Bertsch D, Cagir B. Survival in patients with neuroendocrine tumors of the colon, rectum and small intestine. Am J Surg. 2023;225(1):58-65.
doi pubmed - Huang YQ, Gou R, Diao YS, Yin QH, Fan WX, Liang YP, Chen Y, et al. Charlson comorbidity index helps predict the risk of mortality for patients with type 2 diabetic nephropathy. J Zhejiang Univ Sci B. 2014;15(1):58-66.
doi pubmed - Polee IN, Hermans BCM, van der Zwan JM, Bouwense SAW, Dercksen MW, Eskens F, Havekes B, et al. Long-term survival in patients with gastroenteropancreatic neuroendocrine neoplasms: A population-based study. Eur J Cancer. 2022;172:252-263.
doi pubmed - Xiao G, Xu Z, Zhang Y, Dai S, Ouyang G, Huang Y, Liu Y, et al. The crucial role of age and site in incidence and prognosis of female neuroendocrine neoplasms in the United States: a population-based study from 2000 to 2018. Aging (Albany NY). 2024;16(5):4204-4223.
doi pubmed - White BE, Rous B, Chandrakumaran K, Wong K, Bouvier C, Van Hemelrijck M, George G, et al. Incidence and survival of neuroendocrine neoplasia in England 1995-2018: A retrospective, population-based study. Lancet Reg Health Eur. 2022;23:100510.
doi pubmed - Lian J, Yue Y, Yu W, Zhang Y. Immunosenescence: a key player in cancer development. J Hematol Oncol. 2020;13(1):151.
doi pubmed - Zhang Y, Sun Y, Gan J, Zhou H, Guo S, Wang X, Zhang C, et al. Reconstructing the immunosenescence core pathway reveals global characteristics in pan-cancer. Cancer Immunol Immunother. 2023;72(11):3693-3705.
doi pubmed - Wei Q, Chen R, He X, Qu Y, Yan C, Liu X, Liu J, et al. Multi-omics and single cell characterization of cancer immunosenescence landscape. Sci Data. 2024;11(1):739.
doi pubmed - Hu FH, Feng LP, Jia YJ, Ge MW, Shen LT, Liu P, Chen HL. Frailty and all-cause and cancer-related mortality in cancer patients: A prospective cohort study. Eur J Oncol Nurs. 2024;71:102667.
doi pubmed - Cespedes Feliciano EM, Hohensee C, Rosko AE, Anderson GL, Paskett ED, Zaslavsky O, Wallace RB, et al. Association of prediagnostic frailty, change in frailty status, and mortality after cancer diagnosis in the women's health initiative. JAMA Netw Open. 2020;3(9):e2016747.
doi pubmed - Alamgeer M, Ling RR, Ueno R, Sundararajan K, Sundar R, Pilcher D, Subramaniam A. Frailty and long-term survival among patients in Australian intensive care units with metastatic cancer (FRAIL-CANCER study): a retrospective registry-based cohort study. Lancet Healthy Longev. 2023;4(12):e675-e684.
doi pubmed - Akinoso-Imran AQ, O'Rorke M, Kee F, Jordao H, Walls G, Bannon FJ. Surgical under-treatment of older adult patients with cancer: A systematic review and meta-analysis. J Geriatr Oncol. 2022;13(4):398-409.
doi pubmed - Bertagnolli MM, Singh H. Treatment of older adults with cancer - addressing gaps in evidence. N Engl J Med. 2021;385(12):1062-1065.
doi pubmed - Elkefi S, Choudhury A. Demographic disparities and factors influencing cancer treatment decision-making. J Cancer Educ. 2025.
doi pubmed - Dias LM, Bezerra MR, Barra WF, Rego F. Refusal of medical treatment by older adults with cancer: a systematic review. Ann Palliat Med. 2021;10(4):4868-4877.
doi pubmed - Dorr DA, Markwardt S, Bobo M, Allore HG, Botoseneanu A, Newsom JT, Nagel C, et al. The extent and burden of high multimorbidity on older adults in the US: a descriptive analysis of Medicare beneficiaries. BMC Geriatr. 2024;24(1):777.
doi pubmed - Panigrahi G, Ambs S. How comorbidities shape cancer biology and survival. Trends Cancer. 2021;7(6):488-495.
doi pubmed - Volante M, Grillo F, Massa F, Maletta F, Mastracci L, Campora M, Ferro J, et al. Neuroendocrine neoplasms of the appendix, colon and rectum. Pathologica. 2021;113(1):19-27.
doi pubmed - Ghabi EM, Habib JR, Shoucair S, Javed AA, Sham J, Burns WR, Cameron JL, et al. Detecting somatic mutations for well-differentiated pancreatic neuroendocrine tumors in endoscopic ultrasound-guided fine needle aspiration with next-generation sequencing. Ann Surg Oncol. 2023;30(12):7720-7730.
doi pubmed - Arakelyan J, Zohrabyan D, Philip PA. Molecular profile of pancreatic neuroendocrine neoplasms (PanNENs): Opportunities for personalized therapies. Cancer. 2021;127(3):345-353.
doi pubmed - Chan CS, Laddha SV, Lewis PW, Koletsky MS, Robzyk K, Da Silva E, Torres PJ, et al. ATRX, DAXX or MEN1 mutant pancreatic neuroendocrine tumors are a distinct alpha-cell signature subgroup. Nat Commun. 2018;9(1):4158.
doi pubmed - van Riet J, van de Werken HJG, Cuppen E, Eskens F, Tesselaar M, van Veenendaal LM, Klumpen HJ, et al. The genomic landscape of 85 advanced neuroendocrine neoplasms reveals subtype-heterogeneity and potential therapeutic targets. Nat Commun. 2021;12(1):4612.
doi pubmed - Luchini C, Pantanowitz L, Adsay V, Asa SL, Antonini P, Girolami I, Veronese N, et al. Ki-67 assessment of pancreatic neuroendocrine neoplasms: Systematic review and meta-analysis of manual vs. digital pathology scoring. Mod Pathol. 2022;35(6):712-720.
doi pubmed - Boukhar SA, Gosse MD, Bellizzi AM, Rajan KDA. Ki-67 proliferation index assessment in gastroenteropancreatic neuroendocrine tumors by digital image analysis with stringent case and hotspot level concordance requirements. Am J Clin Pathol. 2021;156(4):607-619.
doi pubmed - Keutgen XM, Nilubol N, Kebebew E. Malignant-functioning neuroendocrine tumors of the pancreas: A survival analysis. Surgery. 2016;159(5):1382-1389.
doi pubmed - Ziogas IA, Schmitz R, Moris D, Vatsaas CJ. The role of surgery for pancreatic neuroendocrine tumors. Anticancer Res. 2022;42(2):629-639.
doi pubmed - Perry RR, Feliberti EC, Hughes MS. Management of pancreatic neuroendocrine tumors: surgical strategies and controversies. Endocr Pract. 2024;30(10):908-916.
doi pubmed - Rinke A, Wittenberg M, Schade-Brittinger C, Aminossadati B, Ronicke E, Gress TM, Muller HH, et al. Placebo-controlled, double-blind, prospective, randomized study on the effect of octreotide LAR in the control of tumor growth in patients with metastatic neuroendocrine midgut tumors (PROMID): results of long-term survival. Neuroendocrinology. 2017;104(1):26-32.
doi pubmed - Caplin ME, Pavel M, Cwikla JB, Phan AT, Raderer M, Sedlackova E, Cadiot G, et al. Lanreotide in metastatic enteropancreatic neuroendocrine tumors. N Engl J Med. 2014;371(3):224-233.
doi pubmed - Shi C, Morse MA. Mechanisms of resistance in gastroenteropancreatic neuroendocrine tumors. Cancers (Basel). 2022;14(24):6114.
doi pubmed - Munteanu C, Schwartz B. The relationship between nutrition and the immune system. Front Nutr. 2022;9:1082500.
doi pubmed - Schoenfeld DA, Moutafi M, Martinez S, Djureinovic D, Merkin RD, Adeniran A, Braun DA, et al. Immune dysfunction revealed by digital spatial profiling of immuno-oncology markers in progressive stages of renal cell carcinoma and in brain metastases. J Immunother Cancer. 2023;11(8):e007240.
doi pubmed - Arends J. Malnutrition in cancer patients: Causes, consequences and treatment options. Eur J Surg Oncol. 2024;50(5):107074.
doi pubmed - Laing E, Gough K, Krishnasamy M, Michael M, Kiss N. Prevalence of malnutrition and nutrition-related complications in patients with gastroenteropancreatic neuroendocrine tumours. J Neuroendocrinol. 2022;34(6):e13116.
doi pubmed - Bossi P, De Luca R, Ciani O, D'Angelo E, Caccialanza R. Malnutrition management in oncology: an expert view on controversial issues and future perspectives. Front Oncol. 2022;12:910770.
doi pubmed - GlobalSurg Collaborative and NIHR Global Health Unit on Global Surgery. Impact of malnutrition on early outcomes after cancer surgery: an international, multicentre, prospective cohort study. Lancet Glob Health. 2023;11(3):e341-e349.
doi pubmed - Menozzi R, Valoriani F, Ballarin R, Alemanno L, Vinciguerra M, Barbieri R, Cuoghi Costantini R, et al. Impact of nutritional status on postoperative outcomes in cancer patients following elective pancreatic surgery. Nutrients. 2023;15(8):1958.
doi pubmed - Clement D, van Leerdam ME, Tesselaar MET, Cananea E, Martin W, Weickert MO, Sarker D, et al. The global leadership into malnutrition criteria reveals a high percentage of malnutrition which influences overall survival in patients with gastroenteropancreatic neuroendocrine tumours. J Neuroendocrinol. 2024;36(4):e13376.
doi pubmed - Das S, Stockton SS, Hassan SA. Carcinoid heart disease management: a multi-disciplinary collaboration. Oncologist. 2023;28(7):575-583.
doi pubmed - Sagastagoitia-Fornie M, Barge-Caballero E, Barge-Caballero G, Couto-Mallon D, Paniagua-Martin MJ, Enriquez-Vazquez D, Blanco-Canosa P, et al. Cancer in patients with heart failure: Incidence, risk factors and prognostic impact. Eur J Intern Med. 2022;105:89-96.
doi pubmed - Tini G, Bertero E, Signori A, Sormani MP, Maack C, De Boer RA, Canepa M, et al. Cancer mortality in trials of heart failure with reduced ejection fraction: a systematic review and meta-analysis. J Am Heart Assoc. 2020;9(18):e016309.
doi pubmed - Taboada RG, Cavalher FP, Rego JF, Riechelmann RP. Tyrosine kinase inhibitors in patients with neuroendocrine neoplasms: a systematic literature review. Ther Adv Med Oncol. 2024;16:17588359241286751.
doi pubmed - Mitchell RJ, Delaney GP, Arnolda G, Liauw W, Lystad RP, Braithwaite J. Survival of patients who had cancer diagnosed through an emergency hospital admission: a retrospective matched case-comparison study in Australia. Cancer Epidemiol. 2024;91:102584.
doi pubmed - Hidalgo Filho CM, Lazar Neto F, Sobottka VP, da Rocha JW, Stangler LTB, Andrade HG, Benfatti Olivato G, et al. Unplanned hospital admissions in patients with solid tumors in Brazil: causes and progressive disease's impact on outcomes. JCO Glob Oncol. 2024;10:e2400063.
doi pubmed - McPhail S, Swann R, Johnson SA, Barclay ME, Abd Elkader H, Alvi R, Barisic A, et al. Risk factors and prognostic implications of diagnosis of cancer within 30 days after an emergency hospital admission (emergency presentation): an International Cancer Benchmarking Partnership (ICBP) population-based study. Lancet Oncol. 2022;23(5):587-600.
doi pubmed - Petrelli F, Ghidini A, Cabiddu M, Perego G, Lonati V, Ghidini M, Oggionni E, et al. Effects of hypertension on cancer survival: A meta-analysis. Eur J Clin Invest. 2021;51(6):e13493.
doi pubmed - Mohammed T, Singh M, Tiu JG, Kim AS. Etiology and management of hypertension in patients with cancer. Cardiooncology. 2021;7(1):14.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
World Journal of Oncology is published by Elmer Press Inc.