| World Journal of Oncology, ISSN 1920-4531 print, 1920-454X online, Open Access |
| Article copyright, the authors; Journal compilation copyright, World J Oncol and Elmer Press Inc |
| Journal website https://wjon.elmerpub.com |
Original Article
Volume 000, Number 000, July 2025, pages 000-000
Association of Low Educational Attainment and Higher Colorectal Cancer Risk: Mediatory Effect of Lifestyle-Associated Factors Within Local Context
Herindita Puspitaningtyasa , Juan Adrian Wiranatab
, Bayu Satria Wiratamac
, Jajah Fachirohd
, Susanna Hilda Hutajulue, f
aDoctorate Program of Health and Medical Science, Faculty of Medicine, Public Health and Nursing, Universitas Gadjah Mada, Yogyakarta, Indonesia
bAcademic Hospital, Universitas Gadjah Mada, Yogyakarta, Indonesia
cDepartment of Biostatistics, Epidemiology, and Population Health, Faculty of Medicine, Public Health, and Nursing, Universitas Gadjah Mada, Yogyakarta, Indonesia
dDepartment of Histology and Cell Biology, Faculty of Medicine, Public Health and Nursing, Universitas Gadjah Mada, Yogyakarta, Indonesia
eDivision of Hematology and Medical Oncology, Department of Internal Medicine, Faculty of Medicine, Public Health and Nursing, Universitas Gadjah Mada/Dr. Sardjito General Hospital, Yogyakarta, Indonesia
fCorresponding Author: Susanna Hilda Hutajulu, Division of Hematology and Medical Oncology, Department of Internal Medicine, Faculty of Medicine, Public Health and Nursing, Universitas Gadjah Mada/Dr. Sardjito General Hospital, Yogyakarta 55284, Indonesia
Manuscript submitted April 24, 2025, accepted June 11, 2025, published online July 8, 2025
Short title: Educational Attainment and CRC Risks
doi: https://doi.org/10.14740/wjon2599
| Abstract | ▴Top |
Background: Educational attainment may influence colorectal cancer (CRC) risks, though the association remains inconclusive. The association might be mediated by health behaviors. This study aimed to explore the association of education on risks of CRC and to elucidate the mediatory effects of lifestyle-associated factors.
Methods: This case-control study included 174 cases and 296 healthy controls. We used a semi-structured questionnaire to collect information on participants’ sociodemographic factors (age, sex, marital status, monthly income, and family history of CRC) and lifestyle-associated behaviors (smoking status, physical activity, and frequency of red meat, legumes, and vegetables intake). Body mass index (BMI) was calculated using body mass measured at first contact. Participants’ education was categorized into those who completed basic education (≥ 12 years) and those who did not complete basic education (< 12 years). Logistic and multiple logistic regression analyses were employed to test the correlation between education and risk of CRC, adjusted by sociodemographic and lifestyle-associated factors. Path analysis was performed to test the mediatory effect of lifestyle-associated behaviors on the correlation.
Results: Participants with lower educational attainment had higher odds of CRC (odds ratio (OR) = 4.76, 95% confidence interval (CI) = 3.07 - 7.38), and the association remained consistent when adjusted by sociodemographic factors (adjusted OR (aOR) = 3.06, 95% CI = 1.86 - 5.03) and combined with lifestyle-associated behaviors (aOR = 2.73, 95% CI = 1.43 - 5.22). The association were consistent among men (OR = 6.14, 95% CI = 3.12 - 12.06; aOR = 4.65, 95% CI = 2.19 - 9.87; aOR = 1.05, 95% CI = 1.02 - 1.09), yet no longer significant among women when adjusted with sociodemographic and lifestyle-associated factors (OR = 3.91, 95% CI = 2.19 - 6.97; aOR = 2.02, 95% CI = 1.02 - 4.00; aOR = 1.56, 95% CI = 0.61 - 3.95). Path analysis showed that the association between educational attainment and risk of CRC was mediated by physical activity, BMI, and intake of red meat, legumes, and vegetables.
Conclusion: In our study, educational attainment was inversely correlated with the odds of CRC and might be mediated by physical activity, BMI, and intake of red meat, legumes, and vegetables. Taking other sociodemographic and lifestyle-associated factors into account, the association between lower educational attainment and higher odds of CRC was more substantial among men. These findings highlight the importance of promoting education and healthy lifestyle behaviors, particularly among men, as an essential part of targeted public health strategies in reducing burden of CRC.
Keywords: CRC; Risk factors; Educational attainment; Lifestyle; Physical activity; Dietary; Path analysis
| Introduction | ▴Top |
Colorectal cancer (CRC) ranks as the fourth most common cancer globally and the third leading cause of cancer-related deaths in both sexes. In Indonesia, it ranked fourth in terms of incidence [1]. In Yogyakarta, the province with the highest cancer prevalence in the country [2], the reported incidence of CRC was 7.4 per 100,000 population [3]. Data from the hospital-based cancer registries (HBCR) at the top referral hospital in the region show that CRC is the second most frequently encountered cancer among patients, only second to breast cancer, with the majority of cases diagnosed at stages III to IV [4].
Risk for cancer may differ among socioeconomic status (SES) groups, with educational attainment being one of the most basic yet important components. Previous studies have shown that people with higher levels of education tend to have more accurate cancer-related knowledge [5] and generally face a lower risk for CRC [6-8]. The lower risk of cancer may be influenced by a range of demographic, behavioral, and biological factors related to higher education attainment (such as more health-conscious dietary behaviors, smoking avoidance, cancer screening participation, and use of hormonal contraception) [9, 10]. Nevertheless, other studies suggest that individuals with higher educational attainment may have an increased risk of CRC. This might be attributed to associated factors such as the consumption of diets linked to CRC risk (e.g., high intake of red meat) and lower occupational levels of physical activity [11-15].
Geographical and sociocultural contexts can further complicate the relationship between educational background and the risk of CRC. In some Asian regions, higher education may be associated with Westernized diets which increase the risk of CRC [16, 17]. Additionally, the food environment, availability and affordability of various foods, which are strongly influenced by geographical location, may outweigh an individual’s nutritional knowledge which was gained through education [18-20]. Regarding physical activity, people with higher education in urban areas may have more sedentary occupations and lifestyles, while those with lower education levels may engage in more physically demanding work [21, 22]. In some urban settings, higher education may also have better access to recreational facilities and greater awareness of the benefits of physical activity. Conversely, access to structured exercise opportunities may be limited in rural areas regardless of educational level [23].
Currently, there is a lack of studies in Indonesia examining the relationship between educational attainment and CRC. Given the complex relationship between educational attainment and the risk of CRC and the importance of sociocultural and geographical context, this study aimed to explore the association between educational attainment and CRC within the Indonesian context.
| Materials and Methods | ▴Top |
Ethical considerations
This study was conducted under ethical approval from the joint ethics committee of the Faculty of Medicine, Public Health, and Nursing of Universitas Gadjah Mada/Dr. Sardjito General Hospital (reference number: KE/FK/0953/EC/2022 and KE/FK/1474/EC/2023). Written informed consent was obtained from all the subjects enrolled in the study. The study was conducted in compliance with the ethical standards of the responsible institution on human subjects as well as with the Helsinki Declaration.
Study participant
We performed a hospital-based case-control study evaluating lifestyle and sociodemographic factors among CRC patients and healthy controls. Recruitments for both cases and controls were performed at the Tulip Integrated Cancer Center, Dr. Sardjito General Hospital, Yogyakarta. Cases were 18 - 75 years old CRC patients, as evidenced by histopathological examination of primary or metastatic tumor tissue following colonoscopy or surgery, with no prior systemic therapy or radiation treatment. All cases were with good performance status (Eastern Cooperative Oncology Group performance status (ECOG PS) ≤ 1). Controls were healthy 18 - 75 years old individuals with no prior history of any malignancy, who visited the clinic as family or guardians of a patient who was not diagnosed with CRC. Subjects were excluded if they were not cooperative, unable to give proper history, or presented with severe comorbidities or terminal illness. Cases with poor performance status were excluded due to possible limitations during interviews and body measurements.
Study variables and measurement
The study used a semi-structured questionnaire to collect sociodemographic and clinical data and assess lifestyle patterns and exposure to CRC risk factors in both case and control groups. Subjects in the case group were asked to recall their history of risk factor exposure for 1 year before diagnosis, while in controls, exposure history was recalled for 1 year before the interview. The questionnaire was divided into sub-sections, which included exploring dietary patterns, smoking history, physical activity, and obesity history of the subjects. The questionnaire was adapted from several sources and studies that included risk factors in the local population.
Sociodemographic information of the subjects included sex, date of birth for age calculation at the time of diagnosis or interview, marital status, education attainment, occupation, and monthly income (in Indonesian Rupiah (IDR)). Educational attainment was categorized into two groups: subjects who had completed mandatory basic education (until senior high school; 12 years) and those who did not finish basic education (< 12 years). Monthly income was categorized into ≥ IDR 3,000,000 and < IDR 3,000,000 based on the National Happiness Index survey in 2021 [24]. Body mass index (BMI) was calculated using body weight as measured using a bioimpedance analysis (BIA) scale at first contact in both groups. Physical activity was stratified into four categories based on mean metabolic equivalent (MET)-hours conversion of subjects’ average activities during 1 week, subjects’ occupation, and sex. Dietary pattern was recorded as subjects’ average consumption of certain food groups within 1 week, categorized into never, less than once a month, 1 - 3 times a month, 1 - 2 times a week, ≥ 3 times a week, and every day. More frequent consumption of red meat and a low intake of vegetables have been largely reported to be associated with a higher risk of CRC. Consumption of nuts and legumes which is one of the common dietary items of the local population has also been correlated with a lower risk of CRC. Taking this into account, we specifically included them in the analysis to reflect the dietary habits of the local population.
Statistical analysis
Descriptive analysis was performed to observe the distribution of subjects’ characteristics. Subject characteristics were summarized using mean and standard deviation (SD), or frequencies, as appropriate. Differences in distribution among groups were confirmed using a t-test and Chi-squared test. Bivariate analysis using logistic regression was then conducted to test the association of educational attainment with CRC. Analysis was followed by multivariate analysis using multiple logistic regression to adjust for sociodemographic and lifestyle-associated factors on the association between education and CRC. Model 2 was adjusted for subjects’ sociodemographic characteristics including age, sex, marital status, monthly income, and family history of CRC. Model 3 was further adjusted for lifestyle-associated factors including physical activity, BMI, smoking status, as well as consumption of red meat, legumes, and vegetables. All categorizations of lifestyle-associated factors were kept in the multivariate analysis.
Path analysis was performed to confirm the mediatory effects of lifestyle-associated factors on the association between education and CRC risk. The correlation of variables in the path diagram with CRC risk was assumed to be linear. Paths with P-value ≥ 0.05 were deleted to correct the model. The bootstrapping confidence interval was performed to check whether the direct, indirect, and total effects, the overall summation of the direct and indirect effects, were statistically significant. Goodness-of-fit of the model was confirmed using root mean square error of approximation (RMSEA), comparative fit index (CFI), and standardized root mean-square residual (SRMR), and the model with the best fit was selected. A P-value of ≤ 0.05 (two-tailed) was considered statistically significant. All statistical analyses were carried out using STATA software version 17 (StataCorp, College Station, TX).
| Results | ▴Top |
Subjects’ characteristics
A total of 470 participants comprising 174 cases and 296 controls were recruited between November 2022 and August 2024. Characteristics of participants are presented in Table 1. Among cases, tumors were detected in the colon in 53 (30.46%) subjects, in the rectosigmoid in 38 (21.84%) subjects, and in the rectum in 83 (47.70%) subjects. Fifty (30.12%) subjects presented with metastasis at diagnosis.
 Click to view | Table 1. Subjects’ Characteristics of CRC Cases and Controls in the Study Population |
Subjects in the case group were older than controls (mean, 55.33 ± 12.99 vs. 43.07 ± 13.89 years, respectively, P < 0.001). The distribution of males and females was not different among the two groups (P = 0.458). In both groups, more subjects were married (P = 0.115). Controls had higher levels of education (P < 0.001) and income (P = 0.014). Controls had higher average BMI (mean, cases 19.83 ± 3.89 vs. controls 25.02 ± 4.86 kg/m2, P < 0.001) and were more physically active compared to cases (P = 0.009). Subjects in the control group had a higher proportion of family history of CRC (P < 0.001). The status of smoking did not differ, with more subjects being non-smokers both in cases and controls (61.49% and 65.54%, respectively, P = 0.377).
Association of educational attainment with CRC
The association of educational attainment with the likelihood of CRC is presented in Table 2. Multiple logistic regression showed that lower education attainment positively correlated with a higher likelihood of CRC, both in the unadjusted model (P < 0.001) and after adjusting for sociodemographic (P < 0.001) and combined with lifestyle-associated factors (P = 0.002). Adjusting for age, sex, marital status, monthly income, and family history of CRC, people who did not complete basic education demonstrated more than three times the odds of CRC compared to those who finished (adjusted odds ratio (aOR) = 3.06, 95% confidence interval (CI) = 1.86 - 5.03). Further adjustments for physical activity, BMI, smoking status, and consumption of red meat, legumes, and vegetables consistently showed that people who did not complete basic education possessed higher odds of CRC compared to those with higher education (aOR = 2.73, 95% CI = 1.43 - 5.22).
 Click to view | Table 2. Association of Education Attainment and Colorectal Cancer Among Group of Men and Women |
Stratification by sex showed that the association between lower educational attainment and higher odds of CRC was consistent. People who did not complete basic education were correlated with a higher likelihood of CRC, both in males (OR = 6.14, 95% CI = 3.12 - 12.06) and females (OR = 3.91, 95% CI = 2.19 - 6.97). However, upon adjustment for sociodemographic and lifestyle-associated factors, a significant association persisted only among males (P < 0.001 and P = 0.002, respectively).
Men with low educational attainment had more than four times the odds of CRC compared with those with higher educational attainment, after adjusting for age, marital status, monthly income, and family history of CRC (aOR = 4.65, 95% CI = 2.19 - 9.87). Further adjustment was done with physical activity, BMI, smoking status, and intake of red meat, legumes, and vegetables. Men who did not complete basic education consistently demonstrated higher odds of CRC compared to those with higher education (aOR = 1.05, 95% CI = 1.02 - 1.09). Similarly, women who did not complete basic education also showed higher odds of CRC compared to those who completed higher education after adjustment for sociodemographic factors (aOR = 2.02, 95% CI = 1.02 - 4.00). Despite not being statistically significant, this association was consistent after further adjustment for lifestyle-associated factors (aOR = 1.56, 95% CI = 0.61 - 3.95).
Mediating effects of lifestyle-associated factors
The hypothesized pathway through which low educational attainment increases the odds of CRC is illustrated in the path diagram presented in Figure 1. The overall goodness-of-fit of the model was acceptable (RMSEA = 0.08, CFI = 0.78, SRMR = 0.07). In the model, low education was associated with physical activity, BMI, and intake of red meat, legumes, and vegetables, which mediated the likelihood of CRC. Low education attainment was also significantly associated with smoking, although it was not dominant in mediating the odds of CRC. In addition to education and its mediating factors, the odds of CRC were influenced by age. As shown in Table 3, low educational attainment had a significant direct effect on the likelihood of CRC (β = 0.175, P < 0.001), as well as an indirect effect via the observed lifestyle-associated risk factors (β = 0.104, P < 0.001), for a total standardized effect of 0.280 (P < 0.001).
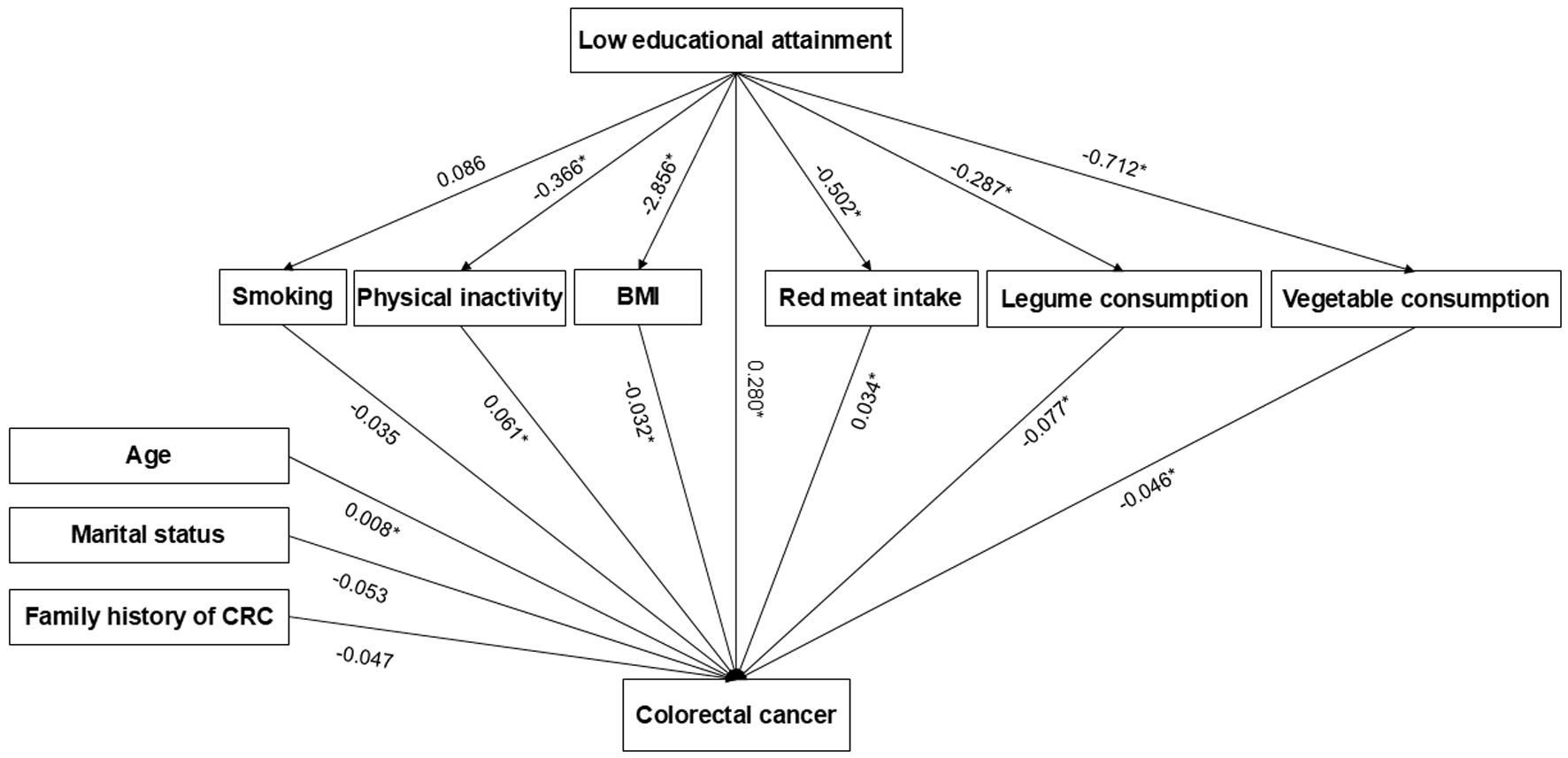 Click for large image | Figure 1. Path analysis diagram of association between low educational attainment and risk of colorectal cancer (RMSEA = 0.08, CFI = 0.78, SRMR = 0.07). Values are reported as standardized estimates. *P-value < 0.05. BMI: body mass index; CFI: comparative fit index; CRC: colorectal cancer; RMSEA: root mean square error of approximation; SRMR: standardized root mean-square residual. |
 Click to view | Table 3. Effect of Low Educational Attainment in Path Analysis of Colorectal Cancer Risk |
| Discussion | ▴Top |
Summary of key findings
This study examined the association between educational attainment and the odds of CRC and explored the mediating effect of lifestyle-associated risk factors on it. In the present study, people with lower education had higher odds of CRC (OR = 4.40, 95% CI = 1.43 - 5.22). Consistent association was demonstrated after adjusting for sociodemographic (aOR = 3.06, 95% CI = 1.86 - 5.03) and combined with lifestyle-associated factors (aOR = 2.73, 95% CI = 1.43 - 5.22). Path analysis results demonstrated that the association between lower education and higher odds of CRC might be mediated by physical activity, BMI, and intake of red meat and vegetables.
Comparison to previous studies
Our findings are consistent with prior studies reporting higher CRC incidence among those with lower educational levels, both in higher- and lower-income countries [8, 25-27]. A study in India reported that the risk of CRC was more than four times higher in people who did not receive 12 years of basic education (OR = 4.47, 95% CI = 1.78 - 11.26) [27]. Another study in the USA also reported that people with less than 12 years of education were associated with a 42% higher risk of CRC [25]. We also showed higher odds of CRC among men who did not complete basic education. The association, however, were no longer significant among women when adjusting for lifestyle-associated factors. A cohort study in the USA reported similar results among men, while the increase in risk was only significant for colon and not rectal cancer among women [7]. Interestingly, a previous study in China showed that lower education was associated with a higher risk of CRC both in men and women [8]. The difference in risk of CRC was influenced both by the biological difference in hormones and genes among men and women, as well as differences in societal attitudes and behaviors [28]. Studies evaluating the association between proinflammatory profile with the risk of CRC were only significant in men, possibly attributed to the healthier lifestyles among women [28, 29].
In our study, low educational attainment was associated with a higher level of physical activity, lower BMI, and lower intake of red meat, legumes, and vegetables. While several studies associated lower educational attainment with a low level of physical activity [30, 31], the inverse correlation observed in this study might be attributable to the subjects’ occupation. People with lower education levels tend to participate in more physically demanding jobs with more time spent at work, which in turn results in a higher level of physical activity [32].
The association between education and BMI has been variedly described in previous studies and was shown to be influenced by other factors such as sex, age, ethnicity, and indices used in the measurements [33-35]. The association observed in our study is in agreement with a recent study using a nationwide longitudinal survey in Indonesia, observing the association between higher educational attainment and higher BMI in the older generation. This study also observed a shift towards a higher risk of obesity among people with lower education due to nutritional transition and diminishing inequality in education among the younger generation [36].
People with lower educational attainment in our study demonstrated lower intake of red meat, legumes, and vegetables. People with higher education generally have better health literacy and have more tendency to practice a healthy diet, attributable to higher socioeconomic status [25, 37-39]. Low education attainment is associated with high carbohydrate and low fiber diets [40]. It is, however, also usually associated with higher consumption of red meats [40].
In this study, being physically inactive and consuming red meat were positively associated with CRC while BMI and consumption of legumes and vegetables were inversely associated with CRC. Previous studies have linked higher levels of physical activity with 25-27% lower risk of CRC, with up to 35% lower risk among people with high BMI [41-43]. Physical activity was known to lower cancer risks through several mechanisms, including decreasing circulating glucose and insulin levels which mitigates hyperinsulinemia, reducing pro-inflammatory cytokines, and improving the immunosurveillance system [44]. Consumption of red meat has been associated with an increased risk of CRC due to the production of carcinogenic substances such as heterocyclic amines (HCAs), polycyclic aromatic hydrocarbons (PAHs), and N-nitroso compounds (NOCs) during its processing at high temperatures [45]. Meanwhile, the consumption of non-starchy vegetables might be protective against CRC due to its potent antioxidative properties which inhibit cell damage and exposure to reactive oxygen species (ROS) [46].
The association between direct effects observed in the path analysis suggests that lower educational attainment may influence the odds of CRC through several interrelated mechanisms beyond lifestyle-associated factors. People with lower education are less likely to participate in CRC screening awareness and to perceive the necessity of preventive health behaviors. Higher education was significantly associated with increased screening uptake [47, 48]. Additionally, lower education was associated with lower health literacy, including awareness of cancer risk factors and symptoms [49]. This serves as a significant barrier to CRC screening, even in the context of accessible services [50].
Strength and limitation
Our study provides additional evidence from the Southeast Asian population, highlighting the importance of educational attainment which not only serves as a socioeconomic indicator but also due to its tangible correlation to risk of CRC. This study combines both multivariable regression and path analysis to confirm the direct and indirect effects of educational attainment on CRC. The inclusion of lifestyle-associated factors provides more insight into the potential mechanism. The study findings may provide a locally relevant perspective on this relationship which may help researchers identify vulnerable populations. Further, policymakers may develop effective, targeted interventions to reduce CRC incidence and improve health outcomes.
Limitations of this study include its case-control design which limits the ability to infer causality. While not as methodologically strong as a cohort study, case-control allows for the identification of associations between exposures and the likelihood of the outcome of interest [51, 52]. Despite this limitation, rigorous data collection and analysis performed ensures the reliability of our findings. These results add to the existing body of evidence and may serve as a basis for further longitudinal or experimental study.
Although hospital-based case-control studies are commonly used in studies on lifestyle-associated risk factors of CRC [53-57], it has inherent limitations in representing the general population. Additionally, our control group may share overlapping risk factors, considering that the majority might have shared genetics and lifestyle with cancer patients. We tried to mitigate this by controlling for family history and known factors associated with CRC risks, including physical activity and dietary patterns, in the multivariate analysis. We also ensured data quality by using an adequate sample size in the study. Notably, the selection of controls in this study reduces the non-response rate and potential differences in data quality with cases, due to the shared experience with cancer patients. This likely results in a higher willingness to provide complete and accurate information [52].
Another limitation of this study is the method of data collection which subjects to recall bias. To reduce this, we included only newly diagnosed cases and minimized the interval between diagnosis, recruitment, and interview to reduce behavioral changes and bias associated with the more distant diagnosis. We limit the recall period to 1 year before diagnosis to allow recollection as objectively as possible and to ensure that the observed results represent the actual pattern of behavior. However, recall bias remains inevitable and should be taken into account when interpreting this result.
Finally, to reduce the risk of confounding factors, we adjusted the multivariate models for known and potential risk factors for CRC, including age, sex, marital status, monthly income, family history of CRC, physical activity, BMI, smoking status, and dietary intake of food groups such as dietary fibers and meats. Nonetheless, the existence of other potential confounders which might influence the observed association was not controlled for.
Conclusions
People who did not finish basic education are three times more likely to have CRC compared to those with higher education. Lower educational attainment was associated with a higher risk of CRC, both directly and indirectly through the mediatory effect of physical activity, BMI, and intake of red meat, legumes and vegetables.
Acknowledgments
The authors thank Norma Dewi Suryani, Fanny Nadila Virginia, Refdiana Dewi, Raden Danang Yulianta, and Yunita for technical assistance.
Financial Disclosure
This study was supported by the Indonesian Ministry of Research, Technology, and Higher Education (2024, grant number: 644/UN1/DITLIT/PT.01.03/2024).
Conflict of Interest
The authors declare no conflict of interest.
Informed Consent
Written informed consent was obtained from the subject of the study for participation in the research.
Author Contributions
Conceptualization: HP, JAW, BSW, JF, SHH. Data acquisition: HP, SHH. Formal analysis and interpretation: HP, BSW, JF. Writing original draft: HP, JAW, SHH. Review and editing draft: HP, JAW, BSW, JF, SHH. All authors have read and agreed to the published version of the manuscript.
Data Availability
The data supporting the findings of this study are available from the corresponding author upon reasonable request.
| References | ▴Top |
- Bray F, Laversanne M, Sung H, Ferlay J, Siegel RL, Soerjomataram I, Jemal A. Global cancer statistics 2022: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2024;74(3):229-263.
doi pubmed - Agency of Health Research and Development. National Report of Basic Health Research 2018. Jakarta; 2019.
- Wiranata JA, Puspitaningtyas H, Hutajulu SH, Fachiroh J, Anggorowati N, Sanjaya GY, Lazuardi L, et al. Temporal and spatial analyses of colorectal cancer incidence in Yogyakarta, Indonesia: a cross-sectional study. Geospat Health. 2023;18(1).
doi pubmed - Jogja Cancer Registry. Report of Dr Sardjito Hospital-based cancer registry in December 2023 [Internet]. 2023 [cited Jan 12, 2024]. Available from: https://canreg.fk.ugm.ac.id/laporan-data/registrasi-kanker-berbasis-rumah-sakit-dr-sardjito-fkkmk-ugm/rkbr-desember-2023/.
- Wilkinson AV, Vasudevan V, Honn SE, Spitz MR, Chamberlain RM. Sociodemographic characteristics, health beliefs, and the accuracy of cancer knowledge. J Cancer Educ. 2009;24(1):58-64.
doi pubmed - Clegg LX, Reichman ME, Miller BA, Hankey BF, Singh GK, Lin YD, Goodman MT, et al. Impact of socioeconomic status on cancer incidence and stage at diagnosis: selected findings from the surveillance, epidemiology, and end results: National Longitudinal Mortality Study. Cancer Causes Control. 2009;20(4):417-435.
doi pubmed - Mouw T, Koster A, Wright ME, Blank MM, Moore SC, Hollenbeck A, Schatzkin A. Education and risk of cancer in a large cohort of men and women in the United States. PLoS One. 2008;3(11):e3639.
doi pubmed - Li L, Fang YJ, Abulimiti A, Huang CY, Liu KY, Chen YM, Zhang CX. Educational level and colorectal cancer risk: the mediating roles of lifestyle and dietary factors. Eur J Cancer Prev. 2022;31(2):137-144.
doi pubmed - Leuven E, Plug E, Ronning M. Education and cancer risk. Labour Econ. 2016;43:106-121.
- Klink U, Mata J, Frank R, Schuz B. Socioeconomic differences in animal food consumption: Education rather than income makes a difference. Front Nutr. 2022;9;993379.
- Aarts MJ, Lemmens VE, Louwman MW, Kunst AE, Coebergh JW. Socioeconomic status and changing inequalities in colorectal cancer? A review of the associations with risk, treatment and outcome. Eur J Cancer. 2010;46(15):2681-2695.
doi pubmed - Wernly S, Semmler G, Schaffler-Schaden D, Flamm M, Aigner E, Datz C, Wernly B. The association between educational status and colorectal neoplasia: results from a screening cohort. Int J Colorectal Dis. 2023;38(1):91.
doi pubmed - Leufkens AM, Van Duijnhoven FJ, Boshuizen HC, Siersema PD, Kunst AE, Mouw T, Tjonneland A, et al. Educational level and risk of colorectal cancer in EPIC with specific reference to tumor location. Int J Cancer. 2012;130(3):622-630.
doi pubmed - Savijarvi S, Seppa K, Malila N, Pitkaniemi J, Heikkinen S. Trends of colorectal cancer incidence by education and socioeconomic status in Finland. Acta Oncol. 2019;58(11):1557-1563.
doi pubmed - Weiderpass E, Pukkala E. Time trends in socioeconomic differences in incidence rates of cancers of gastro-intestinal tract in Finland. BMC Gastroenterol. 2006;6:41.
doi pubmed - Clemente-Suarez VJ, Beltran-Velasco AI, Redondo-Florez L, Martin-Rodriguez A, Tornero-Aguilera JF. Global impacts of western diet and its effects on metabolism and health: a narrative review. Nutrients. 2023;15(12):2749.
doi pubmed - Pingali P. Westernization of Asian diets and the transformation of food systems: Implications for research and policy. Food Policy. 2007;32(3):281-298.
- Thomas TW, Cankurt M. Influence of food environments on dietary habits: insights from a Quasi-Experimental research. Foods. 2024;13(13):2013.
doi pubmed - Nelson Laska M, Larson NI, Neumark-Sztainer D, Story M. Dietary patterns and home food availability during emerging adulthood: do they differ by living situation? Public Health Nutr. 2010;13(2):222-228.
doi pubmed - WHO. Diet, nutrition and the prevention of chronic diseases. Geneva, Switzerland: WHO; 2002.
- Puciato D. Sociodemographic associations of physical activity in people of working age. Int J Environ Res Public Health. 2019;16(12):2134.
doi pubmed - Shaw BA, Spokane LS. Examining the association between education level and physical activity changes during early old age. J Aging Health. 2008;20(7):767-787.
doi pubmed - Hansen AY, Hartley D. Promoting Active Living in Rural Communities. San Diego, CA; 2015.
- Suchaini U, Nugraha WPS, Dwipayana IKD, Lestari SA. Happiness Index 2021. Widianto T, Apriyanto A, Jamilah, editors. Jakarta, Indonesia: BPS - Statistics Indonesia; 2021.
- Doubeni CA, Laiyemo AO, Major JM, Schootman M, Lian M, Park Y, Graubard BI, et al. Socioeconomic status and the risk of colorectal cancer: an analysis of more than a half million adults in the National Institutes of Health-AARP Diet and Health Study. Cancer. 2012;118(14):3636-3644.
doi pubmed - Robertson NM, Burus T, Hudson L, Hull PC, Park L, Vanderford NL. Lung and colorectal cancer disparities in Appalachian Kentucky: spatial analysis on the influence of education and literacy. Int J Environ Res Public Health. 2023;20(14):6363.
doi pubmed - Ferreira AM, Chodankar SU, Vaz FS, D'Souza D B, Kulkarni MS. Risk factors for colorectal cancer in Goa, India: a hospital-based case-control study. Indian J Community Med. 2021;46(3):474-478.
doi pubmed - Choi Y, Kim N. Sex difference of colon adenoma pathway and colorectal carcinogenesis. World J Mens Health. 2024;42(2):256-282.
doi pubmed - Jakszyn P, Cayssials V, Buckland G, Perez-Cornago A, Weiderpass E, Boeing H, Bergmann MM, et al. Inflammatory potential of the diet and risk of colorectal cancer in the European Prospective Investigation into Cancer and Nutrition study. Int J Cancer. 2020;147(4):1027-1039.
doi pubmed - Kari JT, Viinikainen J, Bockerman P, Tammelin TH, Pitkanen N, Lehtimaki T, Pahkala K, et al. Education leads to a more physically active lifestyle: Evidence based on Mendelian randomization. Scand J Med Sci Sports. 2020;30(7):1194-1204.
doi pubmed - Scholes S, Bann D. Education-related disparities in reported physical activity during leisure-time, active transportation, and work among US adults: repeated cross-sectional analysis from the National Health and Nutrition Examination Surveys, 2007 to 2016. BMC Public Health. 2018;18(1):926.
doi pubmed - Cusatis R, Garbarski D. Different domains of physical activity: The role of leisure, housework/care work, and paid work in socioeconomic differences in reported physical activity. SSM Popul Health. 2019;7:100387.
doi pubmed - von Hippel PT, Lynch JL. Why are educated adults slim-Causation or selection? Soc Sci Med. 2014;105:131-139.
doi pubmed - Witkam R, Gwinnutt JM, Humphreys J, Gandrup J, Cooper R, Verstappen SMM. Do associations between education and obesity vary depending on the measure of obesity used? A systematic literature review and meta-analysis. SSM Popul Health. 2021;15:100884.
doi pubmed - Benson R, von Hippel PT, Lynch JL. Does more education cause lower BMI, or do lower-BMI individuals become more educated? Evidence from the National Longitudinal Survey of Youth 1979. Soc Sci Med. 2018;211:370-377.
doi pubmed - Liwin LK. Shifting educational gradients in body mass index trajectories of Indonesians: an age period cohort analysis. BMC Public Health. 2022;22(1):1004.
doi pubmed - Sandri E, Pardo J, Cantin Larumbe E, Cerda Olmedo G, Falco A. Analysis of the influence of educational level on the nutritional status and lifestyle habits of the young Spanish population. Front Public Health. 2024;12:1341420.
doi pubmed - Zarnowski A, Jankowski M, Gujski M. Public awareness of diet-related diseases and dietary risk factors: a 2022 nationwide cross-sectional survey among adults in Poland. Nutrients. 2022;14(16):3285.
doi pubmed - Nishinakagawa M, Sakurai R, Nemoto Y, Matsunaga H, Takebayashi T, Fujiwara Y. Influence of education and subjective financial status on dietary habits among young, middle-aged, and older adults in Japan: a cross-sectional study. BMC Public Health. 2023;23(1):1230.
doi pubmed - Azizi Fard N, De Francisci Morales G, Mejova Y, Schifanella R. On the interplay between educational attainment and nutrition: a spatially-aware perspective. EPJ Data Sci. 2021;10(1):18.
- Eaglehouse YL, Koh WP, Wang R, Aizhen J, Yuan JM, Butler LM. Physical activity, sedentary time, and risk of colorectal cancer: the Singapore Chinese Health Study. Eur J Cancer Prev. 2017;26(6):469-475.
doi pubmed - Boyle T, Keegel T, Bull F, Heyworth J, Fritschi L. Physical activity and risks of proximal and distal colon cancers: a systematic review and meta-analysis. J Natl Cancer Inst. 2012;104(20):1548-1561.
doi pubmed - Shaw E, Farris MS, Stone CR, Derksen JWG, Johnson R, Hilsden RJ, Friedenreich CM, et al. Effects of physical activity on colorectal cancer risk among family history and body mass index subgroups: a systematic review and meta-analysis. BMC Cancer. 2018;18(1):71.
doi pubmed - Larson EA, Dalamaga M, Magkos F. The role of exercise in obesity-related cancers: Current evidence and biological mechanisms. Semin Cancer Biol. 2023;91:16-26.
doi pubmed - Ashari LS, Abd Rashid AA, Mohd Razif S, Yeong Yeh L, Jan Mohamed HJ. Diet is linked to colorectal cancer risk among Asian adults: a scoping review. Malays J Med Sci. 2023;30(3):8-31.
doi pubmed - Zhou E, Rifkin S. Colorectal cancer and diet: risk versus prevention, is diet an intervention? Gastroenterol Clin North Am. 2021;50(1):101-111.
doi pubmed - Jiang S, Velasquez-Garcia H. The role of education in colorectal cancer screening participation: Updated evidence from Canadian Community Health Survey (2011–2012). Cancer Treat Res Commun. 2017;10:1-5.
- Hermann S, Friedrich S, Haug U, Rohrmann S, Becker N, Kaaks R. Association between socioeconomic and demographic characteristics and utilization of colonoscopy in the EPIC-Heidelberg cohort. Eur J Cancer Prev. 2015;24(2):81-88.
doi pubmed - Hvidberg L, Pedersen AF, Wulff CN, Vedsted P. Cancer awareness and socio-economic position: results from a population-based study in Denmark. BMC Cancer. 2014;14:581.
doi pubmed - Chan TK, Tan LWL, van Dam RM, Seow WJ. Cancer screening knowledge and behavior in a multi-ethnic Asian population: the singapore community health study. Front Oncol. 2021;11:684917.
doi pubmed - Singh H, Mahmud SM. Different study design in the epidemiology of cancer: case-control vs. cohort studies. In: Verma M, editor. Methods in molecular biology, cancer epidemiology. Totowa, NJ: Humana Press; 2009. (Methods in Molecular Biology; vol. 471).
- dos Santos Silva I. Cancer epidemiology: principles and methods. Lyon, France: International Agency for Research on Cancer; 1999.
- Yarmand S, Abdollahi N, Nejad ET, Souni F, Vali M, Nouri M, Shateri Z, et al. Association between adherence to a dietary approach to stop hypertension and the Mediterranean diets and risk of colorectal cancer: A matched case-control study. Clin Nutr ESPEN. 2024;60:195-202.
doi pubmed - Nejad ET, Moslemi E, Souni F, Mahmoodi M, Vali M, Vatanpour M, Nouri M, et al. The association between pro-vegetarian dietary pattern and risk of colorectal cancer: a matched case-control study. BMC Res Notes. 2023;16(1):326.
doi pubmed - Quang N, Hien NQ, Quang NT, Chung NT. Active lifestyle patterns reduce the risk of colorectal cancer in the north of Vietnam: a hospital-based case-control study. Cancer Control. 2019;26(1):1073274819864666.
doi pubmed - Chen Q, Li K, Liu Y, Yu X, Ou F. Association of body composition indicators with colorectal cancer: a hospital-based case-control study. J Cancer Res Clin Oncol. 2024;150(7):344.
doi pubmed - Shafiee NH, Razalli NH, Shahril MR, Muhammad Nawawi KN, Mohd Mokhtar N, Abd Rashid AA, Ashari LS, et al. Dietary inflammatory index, obesity, and the incidence of colorectal cancer: findings from a hospital-based case-control study in Malaysia. Nutrients. 2023;15(4):982.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
World Journal of Oncology is published by Elmer Press Inc.