| World Journal of Oncology, ISSN 1920-4531 print, 1920-454X online, Open Access |
| Article copyright, the authors; Journal compilation copyright, World J Oncol and Elmer Press Inc |
| Journal website https://wjon.elmerpub.com |
Case Report
Volume 16, Number 4, August 2025, pages 422-425
Breast Cancer With Airway Edema Caused by Metastatic Fracture of the Cervical Vertebra
Daigo Suzukia, b, Masanori Oshib, c, Aya Nishikawad, Kei Kawashimab, c, Mahato Sasamotob, c, Yukako Shibatad, Syoko Adachid, Kazutaka Naruid, Hiroki Takasee, f, Akimitsu Yamadab, c, g, Satoshi Fujiie, f, Itaru Endob, c
aSchool of Medicine, Yokohama City University, Kanagawa, Japan
bDepartment of Breast Surgery, Yokohama City University Hospital, Kanagawa, Japan
cDepartment of Gastroenterological Surgery, Yokohama City University Graduate School of Medicine, Kanagawa, Japan
dDepartment of Breast and Thyroid Surgery, Yokohama City University Medical Center, Kanagawa, Japan
eDepartment of Molecular Pathology, Yokohama City University Hospital, Kanagawa, Japan
fDepartment of Pathology, Yokohama City University Hospital, Kanagawa, Japan
gCorresponding Author: Akimitsu Yamada, Department of Gastroenterological Surgery, Yokohama City University Graduate School of Medicine, Yokohama City, Kanagawa 236-0004, Japan
Manuscript submitted March 18, 2025, accepted June 20, 2025, published online July 8, 2025
Short title: Airway Edema From Breast Cancer Metastasis
doi: https://doi.org/10.14740/wjon2575
| Abstract | ▴Top |
Bone is a common site of breast cancer metastasis, with the spine showing a particularly high affinity. An 83-year-old Japanese woman with Alzheimer’s disease presented with a palpable mass in her left breast. A needle biopsy revealed invasive ductal carcinoma of the breast, hormone receptor-positive, human epidermal growth factor receptor 2 (HER2)-negative, with lymph node metastasis. Chest dynamic computed tomography showed no distant metastases. She was diagnosed with luminal-type, stage IIB (T2N1M0) breast cancer and underwent surgery. During induction of general anesthesia, intubation was difficult due to airway edema, necessitating bronchoscopy. The day after surgery, she reported neck pain, and radiography revealed a compression fracture of the third cervical vertebra. Magnetic resonance imaging confirmed a metastatic lesion in the third cervical vertebra. Postoperatively, she received endocrine therapy with letrozole, radiation therapy with zoledronic acid, and a cervical collar for cervical metastases. Seven months later, the osteolytic lesion calcified, and her pain improved. This case is unique because solitary cervical vertebral metastases from breast cancer, leading to compression fractures and airway edema, are rare. The case highlights the importance of considering cervical metastases in patients with breast cancer who develop airway difficulties or unexplained neck pain, particularly in the perioperative setting. Early recognition and intervention are crucial for preventing complications and optimizing patient outcomes.
Keywords: Breast cancer; Airway edema; Alzheimer’s disease; Cervical vertebra fracture; Prevertebral soft tissue swelling
| Introduction | ▴Top |
Bone is a common site for breast cancer metastasis, with the spine being a particularly frequent site of metastasis. More than 70% of patients with breast cancer and bone metastasis experience spinal involvement [1]. However, reports of isolated cervical vertebral metastasis leading to fractures with airway edema are rare. Breast cancer metastasis is often detected upon symptom onset; however, these symptoms may be masked by various comorbidities associated with aging. Therefore, healthcare providers should remain vigilant and exercise caution in clinical practice.
| Case Report | ▴Top |
An 83-year-old woman with Alzheimer’s disease presented to our hospital with a mass in her left breast. Her medical history included osteoporosis, a lumbar spine compression fracture, and Alzheimer’s disease (geriatric assessment G8 score: 6, performance status: 3). Her family history was notable for breast cancer in her daughter and skin cancer in her son. Palpation revealed a mass approximately 3 cm in size in the upper region and an enlarged axillary lymph node. No changes were observed in the skin overlying the mass. The patient’s orientation was limited to stating her name and following simple instructions. Therefore, obtaining detailed symptom information through a standard medical interview was challenging. Ultrasonography showed an irregular hypoechoic lesion measuring 25.0 × 10.2 × 32.3 mm at the 12 o’clock position in the left upper region, and an enlarged lymph node measuring 31.2 × 28.8 mm in the left axilla, with partially fluid-filled components and abundant blood flow. Blood tests revealed elevated D-dimer (2.78 µg/mL; normal range: < 1.0 µg/mL) and a normal bone resorption marker, tartrate-resistant acid phosphatase 5b (TRAP 5b), 287 mU/mL (female baseline: 120 - 420 mU/mL). Breast cancer markers were elevated: carcinoembryonic antigen (CEA), 3.4 ng/mL (normal range: 0 - 5.0 ng/mL); cancer antigen 15-3 (CA15-3), 52.1 U/mL (normal range: < 25 U/mL). Pathological examination from needle biopsy for the breast tumor demonstrated invasive tumor cells that formed cord-like or nest-like structures. The tumor status was as follows: estrogen receptor (ER)-positive (Allred score 8); progesterone receptor (PgR)-positive (Allred score 8); human epidermal growth factor receptor 2 (HER2)-negative (1+); Ki-67, 18.1%; nuclear grade, 2; histological grade, II. Axillary lymph node biopsy revealed overlapping clusters of atypical cells, suggesting metastasis of breast cancer. Dynamic computed tomography (CT) of the breast revealed multiple diffuse contrast-enhancing nodules in the left breast and a 30-mm enlarged lymph node at level I of the left axilla. No enlarged lymph nodes were noted at levels II or III of the axillae, and no distant metastases were observed. The upper cervical spine was not included in the imaging range of the preoperative chest CT; therefore, cervical metastasis could not be diagnosed preoperatively. Bone scintigraphy was not performed because there were no preoperative findings suggestive of bone metastasis. Magnetic resonance imaging (MRI) was not performed. The patient was diagnosed with luminal-type invasive ductal carcinoma, cT2N1M0, and stage IIB breast cancer. Considering her age and performance status, she was scheduled for left mastectomy and axillary lymph node dissection prior to initiating medication therapy. Airway edema was observed upon the induction of general anesthesia, making endotracheal intubation difficult. The anesthesiologist considered anaphylaxis, upper respiratory tract infection, and mechanical irritation from intubation attempts as differential diagnoses, but determined that mask ventilation was possible and there was no need to discontinue anesthesia. The patient was intubated under bronchoscopy, which enabled the surgical procedure to be completed safely. Postoperatively, a detailed interview with the patient’s daughter regarding the difficulty in intubation revealed that the patient had complained of persistent neck pain prior to admission. A detailed medical interview and physical examination revealed tenderness near the left sternocleidomastoid muscle. No neurological abnormalities or additional tenderness were observed. On the first postoperative day, cervical MRI revealed the presence of bone metastasis at the third cervical vertebra (Fig. 1a). Neck radiography showed a compression fracture of the same location (Fig. 1b). The patient was treated with a cervical collar, radiation therapy (8 Gray/1 fraction), and zoledronic acid. Seven months after treatment initiation, follow-up cervical radiography showed osteosclerosis at the lesion site (Fig. 1c), and the cervical collar was removed. The patient is currently undergoing oral letrozole therapy with bone modifying agents as an outpatient. Several guidelines suggest using CDK4/6 inhibitor adding to aromatase inhibitor as a first-line treatment for metastatic ER+/HER2- breast cancer. After discussing with the family the potential benefits, such as improved prognosis, as well as the disadvantages, including adverse events, frequency of hospital visits, and medical costs, the patient’s family opted for treatment with an aromatase inhibitor alone.
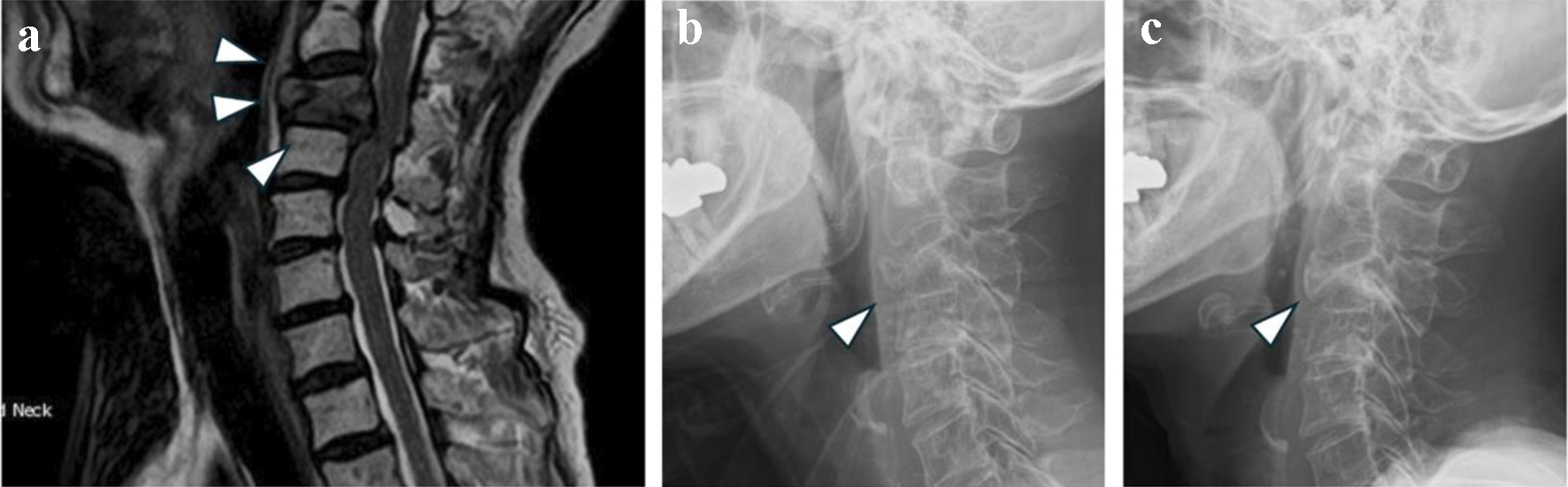 Click for large image | Figure 1. (a) Cervical MRI performed on postoperative day 1. Low signal intensity area existed in the third cervical vertebra (arrowheads). (b) Neck X-ray taken on postoperative day 1. The third cervical vertebra was collapsed (arrowhead). (c) Cervical spine X-ray taken 7 months after the initiation of neck lesion treatment. Osteosclerosis appeared in the third cervical vertebra (arrowhead). MRI: magnetic resonance imaging. |
| Discussion | ▴Top |
Bone metastasis occurred in approximately 69% of patients dying with breast cancer between the 1960s and the 1990s [1]. However, in recent years, its incidence has decreased by approximately 4.1-30% due to advancements in early detection technologies and treatment methods [2]. Vertebrae are a common site of bone metastasis, and more than 70% of breast cancer patients with bone metastasis have spinal involvement [3]. Hematogenous spread is the most common pathway for bone metastasis, and the vertebral venous plexus plays a critical role. Due to its low pressure, large volume, slow blood flow, and abundant vascular branches, tumor cells can easily transfer to nearby bones [4]. However, cervical vertebrae account for only 3% of the first metastases, a proportion lower than that observed in other axial bones of the body [5]. This lower incidence is attributed to the role of the vertebral venous plexus, which facilitates isolated vertebral metastasis from breast cancer. Consequently, the initial site of breast cancer metastasis is typically in the thoracic vertebrae, which are anatomically adjacent [4].
Solitary bone metastasis is rare. Niikura et al reported that solitary metastasis occurred in 87 of 351 female breast cancer patients with bone-only metastasis [6]. Furthermore, solitary bone metastasis associated with fractures is uncommon; however, in the case of vertebral metastasis, bone-only metastasis is reportedly a risk factor for fractures within a short period [7]. Dibekoglu et al reported that 41 (29.5%) of 139 breast cancer patients with solitary bone metastases experienced fractures, of which 26 (63.4%) had spinal fractures [8]. Bone metastasis is typically diagnosed in clinical practice after the appearance of symptoms such as pain, prompting further investigation. By the time symptoms manifest, the disease is often already advanced, with metastasis to other sites frequently present. Cancer-secreted interleukin (IL)-1, IL-6, and IL-11 have been found to increase osteoclast activation. These cytokines are involved in the interaction that plays a significant role in osteoclast development and activity. Increased osteoclast activity subsequently creates a bone microenvironment that favors cancer cell metastasis, growth, and development [9]. Therefore, solitary bone metastases are rare.
The mechanism of airway edema in our case was thought to be prevertebral soft tissue swelling associated with cervical vertebral metastasis. The anterior portion of the cervical spine contains spaces such as the posterior pharyngeal space and anterior vertebral space, as well as muscles and fascia such as the rectus capitis anterior, rectus capitis lateralis, longus capitis, and longus colli muscles [10]. Prevertebral soft tissue swelling is caused by hematoma and edema resulting from injury to these structures due to vertebral fractures [11]. This phenomenon has been reported to occur more frequently in odontoid fractures, compression fractures, hyperextension injuries [12], and injuries to prevertebral elements such as vertebral bodies [12]. Cleiman et al reported a case of complete airway obstruction caused by prevertebral soft tissue swelling due to a cervical vertebral fracture [13].
In our case, bone metastases could not be detected preoperatively but were revealed through careful interviews with the patient’s family after the intubation difficulty due to airway edema. The failure to detect bone metastasis preoperatively can be attributed to the fact that the third cervical vertebra was outside the range of dynamic CT of the breast at our hospital and the patient’s Alzheimer’s disease impaired her ability to express her disease status. Pain assessment scales commonly used for elderly patients with comorbidities such as Alzheimer’s disease are unreliable [14], and impairment of the ability to report pain may delay the expression of symptoms [15]. Beach et al conducted an experiment using a facial movement coding system to evaluate changes in facial expressions related to pain in patients with Alzheimer’s disease. This experiment revealed that significant pain could be detected regardless of the severity of Alzheimer’s disease [16]. In our case, it is regrettable that a history of the patient’s neck pain could not be obtained from the family prior to surgery, which prevented further investigations from being conducted. However, such objective pain assessment may have been useful in detecting the patient’s pain.
We report a rare case of solitary breast cancer metastasis to the cervical spine that was difficult to diagnose preoperatively, resulting in a compression fracture and airway edema. Airway edema caused by the cervical vertebral fracture was conceivably due to prevertebral soft tissue swelling resulting from the metastatic bone fracture. This case leads us to conclude that detecting symptoms in patients who have difficulty expressing their condition, such as those with dementia, requires a comprehensive approach involving collaboration with family members, caregivers, and multiple healthcare professionals. When direct communication with the patient is limited, healthcare providers should gather information from various sources including family members, caregivers, medical records, referral letters, and medication histories. Additionally, careful observation of the patient’s behavior and facial expressions, along with appropriate cognitive function tests when indicated, can provide valuable insights for comprehensive patient assessment.
Acknowledgments
None to declare.
Financial Disclosure
None to declare.
Conflict of Interest
The authors declare that they have no conflict of interest.
Informed Consent
Consent was obtained from the patient for participation in this study.
Author Contributions
DS reviewed the literature and wrote the manuscript. HT and SF contributed to the pathological diagnosis. AY, AN, KK, KN, MO, MS, YS, SA, and IE reviewed the manuscript. All the authors have read and approved the final version of the manuscript.
Data Availability
The authors declare that data supporting the findings of this study are available within the article.
Abbreviations
ER: estrogen receptor; HER2: human epidermal growth factor receptor 2; PgR: progesterone receptor
| References | ▴Top |
- Coleman RE, Rubens RD. The clinical course of bone metastases from breast cancer. Br J Cancer. 1987;55(1):61-66.
doi pubmed - Zhang H, Zhu W, Biskup E, Yang W, Yang Z, Wang H, Qiu X, et al. Incidence, risk factors and prognostic characteristics of bone metastases and skeletal-related events (SREs) in breast cancer patients: A systematic review of the real world data. J Bone Oncol. 2018;11:38-50.
doi pubmed - Pan Y, Lin Y, Mi C. Clinicopathological characteristics and prognostic risk factors of breast cancer patients with bone metastasis. Ann Transl Med. 2021;9(16):1340.
doi pubmed - Zhu M, Liu X, Qu Y, Hu S, Zhang Y, Li W, Zhou X, et al. Bone metastasis pattern of cancer patients with bone metastasis but no visceral metastasis. J Bone Oncol. 2019;15:100219.
doi pubmed - Tian M, Zhao J, Mi X, Wang K, Kong D, Mao H, Wang T. Progress in research on effect of PM(2.5) on occurrence and development of atherosclerosis. J Appl Toxicol. 2021;41(5):668-682.
doi pubmed - Niikura N, Liu J, Hayashi N, Palla SL, Tokuda Y, Hortobagyi GN, Ueno NT, et al. Treatment outcome and prognostic factors for patients with bone-only metastases of breast cancer: a single-institution retrospective analysis. Oncologist. 2011;16(2):155-164.
doi pubmed - Plunkett TA, Smith P, Rubens RD. Risk of complications from bone metastases in breast cancer. implications for management. Eur J Cancer. 2000;36(4):476-482.
doi pubmed - Dibekoglu C, Turanli S, Karaman N, Ozcelik KC, Erdogan O. Bone fracture in breast cancer patients with isolated bone metastasis. Chirurgia (Bucur). 2015;110(1):43-48.
pubmed - Wan X, Mo H, Chen J, Zhou Q, Qiu S, Zou Y, Wu W, et al. Risk factors for brain metastasis in lung cancer: an umbrella review of systematic reviews and meta-analyses. BMJ Open. 2025;15(1):e087181.
doi pubmed - McDavid LJ, Khan YS. Anatomy, head and neck, prevertebral muscles. In: StatPearls. Treasure Island (FL) ineligible companies. 2025.
pubmed - Dai LY. Significance of prevertebral soft tissue measurement in cervical spine injuries. Eur J Radiol. 2004;51(1):73-76.
doi pubmed - Templeton PA, Young JW, Mirvis SE, Buddemeyer EU. The value of retropharyngeal soft tissue measurements in trauma of the adult cervical spine. Cervical spine soft tissue measurements. Skeletal Radiol. 1987;16(2):98-104.
doi pubmed - Cleiman P, Nemeth J, Vetere P. A significant cervical spine fracture: think of the airway. J Emerg Med. 2012;42(2):e23-25.
doi pubmed - Pickering G, Eschalier A, Dubray C. Pain and Alzheimer's disease. Gerontology. 2000;46(5):235-241.
doi pubmed - Anderson AR, Iversen WL, Carter MA, Moss KO, Cowan RL, Monroe TB. Experimentally evoked pain in Alzheimer's disease. J Am Assoc Nurse Pract. 2021;34(1):18-25.
doi pubmed - Beach PA, Huck JT, Miranda MM, Foley KT, Bozoki AC. Effects of Alzheimer disease on the facial expression of pain. Clin J Pain. 2016;32(6):478-487.
doi pubmed
This article is distributed under the terms of the Creative Commons Attribution Non-Commercial 4.0 International License, which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
World Journal of Oncology is published by Elmer Press Inc.